CARACTERIZAÇÃO DAS HOSPITALIZAÇÕES POR MALFORMAÇÕES CONGÊNITAS DO APARELHO CIRCULATÓRIO EM CRIANÇAS MENORES DE UM ANO
Characterization of hospitalizations for circulatory system congenital malformations appliance in children under one year old
Caracterización de hospitalizaciones por malformaciones congénitas del sistema circulatorio en niños menores de un año
Elisângela de Fraga Vidal - Enfermeira do Hospital da Criança Santo Antônio da Santa de Casa de Misericórdia de Porto Alegre (SCMPA). Mestranda do Programa de Pós-Graduação em Enfermagem (PPGEnf) - Mestrado Profissional da Universidade Federal de Ciências daSaúde de Porto Alegre (UFCSPA). Membro do Grupo de Pesquisa Tecnologia, Gestão, Educação e Segurança no Trabalho (TeGEST) da UFCSPA. ORCID: 0000-0002-0766-9896
Aléxia Garcês Maciel - Acadêmica do Curso de Bacharelado em Enfermagem da UFCSPA. Bolsista de Iniciação Científica. Membro do TeGEST da UFCSPA. ORCID: 0000-0001-6271-4875
Nathália Bottega Banaletti - Acadêmica do Curso de Bacharelado em Enfermagem da UFCSPA.Bolsista de Iniciação Científica Voluntária. Membro do TeGEST da UFCSPA. ORCID: 0000-0002-9142-0558
Perla Adriana Di Leone - Enfermeira. Professora da Universidade Luterana do Brasil (ULBRA) - Canoas. ORCID: 0000-0001-6765-4947
Lucia Campos Pellanda - Médica. Doutora em Ciências da Saúde. Professora Titular do Departamento de Saúde Coletiva da UFCSPA. ORCID: 0000-0002-8776-2248
Gisele Pereira de Carvalho - Enfermeira. Doutora em Clínica Médica e Ciências da Saúde.Professora Adjunto do Departamento de Enfermagem. Membro do TeGEST da UFCSPA. ORCID: 0000-0003-1258-4552
Adriana Aparecida Paz - Enfermeira. Doutora em Enfermagem. Professora Adjunto do Departamento de Enfermagem.Docente permanente no PPG-Enf da UFCSPA. Líder do TeGEST da UFCSPA. ORCID: 0000-0002-1932-2144
Resumo
Objetivo: Caracterizar as internações hospitalares por malformações congênitas do aparelho circulatório em crianças menores de um ano no Brasil, Rio Grande do Sul e Porto Alegre. Método: Estudo de série histórica com informações disponibilizadas por bancos de dados de acesso públicos, no período de 2016 a 2020. Resultados: Porto Alegre é referência no atendimento das malformações congênitas, sendo ⅘ das internações provenientes de outros municípios. Predomina o atendimento em caráter de urgência. A média de permanência e a taxa de mortalidade em Porto Alegre são superiores em comparação às do estado e país, com taxa de mortalidade 29,39% maior para crianças não residentes em Porto Alegre. Conclusão: Porto Alegre tem mortalidade e permanência altas por receber casos complexos de todo o estado. É possível que investimentos em hospitais regionais, recursos tecnológicos, transporte e educação modifiquem o padrão de referência e reduzam a taxa de mortalidade e a permanência hospitalar.
DESCRITORES: Cardiopatias Congênitas; Pesquisa sobre Serviços de Saúde; Doenças e Anormalidades Congênitas, Hereditárias e Neonatais; Saúde da Criança; Indicadores de Morbimortalidade.
ABSTRACT
Objective: To characterize hospitalizations due to congenital malformations of the circulatory system in children under one year old in Brazil, Rio Grande do Sul and Porto Alegre. Method: Historical series study with information made available by publicly accessible databases, from 2016 to 2020. Results: Porto Alegre is a reference in the care of congenital malformations, with ⅘ of hospitalizations coming from other municipalities. Emergency care predominates. The average length of stay and the mortality rate in Porto Alegre are higher compared to the state and country, with a mortality rate 29.39% higher for children not residing in Porto Alegre. Conclusion: Porto Alegre has high mortality and length of stay because it receives complex cases from all over the state. It is possible that investments in regional hospitals, technological resources, transport and education will modify the reference pattern and reduce the mortality rate and hospital stay.
DESCRIPTORS: Congenital Heart Diseases; Research on Health Services; Congenital, Hereditary and Neonatal Diseases and Abnormalities; Child Health; Morbimortality Indicators.
RESUMEN
Objetivo: Caracterizar los ingresos hospitalarios por malformaciones congénitas del sistema circulatorio en niños menores de un año en Brasil, Rio Grande do Sul y Porto Alegre. Método: Estudio de series temporales con información proporcionada por bases de datos de acceso público, de 2016 a 2020. Resultados: Porto Alegre es referencia en la atención de malformaciones congénitas, con ⅘ de las hospitalizaciones provenientes de otros municipios. Predomina la atención de urgencias. La estancia media y la tasa de mortalidad en Porto Alegre son superiores a las del estado y del país, con una tasa de mortalidad 29,39% superior para los niños no residentes en Porto Alegre. Conclusión: Porto Alegre tiene alta mortalidad y estancia debido a la recepción de casos complejos de todo el estado. Es posible que inversiones en hospitales regionales, recursos tecnológicos, transporte y educación puedan cambiar el patrón de derivación y reducir la tasa de mortalidad y la estancia hospitalaria.
DESCRIPTORES: Cardiopatías Congénitas; Investigación en Servicios de Salud; Enfermedades y Anomalías Congénitas, Hereditarias y Neonatales; Salud Infantil; Indicadores de Morbilidad y Mortalidad.
INTRODUÇÃO
As cardiopatias congênitas (CC) são malformações cardiovasculares, com elevado risco de morte em ausência de diagnóstico e tratamento precoce.(1-2) Majoritariamente graves, destacam-se as mais complexas: coarctação da aorta, tetralogia de Fallot, síndrome do coração esquerdo hipoplásico, atresia pulmonar, retorno venoso pulmonar anômalo total, transposição das grandes artérias e truncus arteriosus(3), as quais necessitam assistência especializada e demandam abordagem cirúrgica no primeiro ano de vida do recém-nascido(3), cabendo ao enfermeiro especialista prover a assistência qualificada e segura a essas crianças na Unidade de Tratamento Intensivo Pediátrica (UTIP) ou Neonatal (UTIN).
Nesse sentido, a criança com CC necessitará de internação clínico/cirúrgica para intervenção. Os registros das hospitalizações no Sistema Único de Saúde (SUS) por malformações cardíacas congênitas (MCC) são disponibilizados no Sistema de Informações Hospitalares (SIH) do SUS gerenciado pelo Departamento de Informática do Sistema Único de Saúde (DATASUS). Diante desses recursos informativos, é possível conhecer o perfil epidemiológico dos usuários do SUS, permitindo a elaboração de políticas públicas e a implementação de novas tecnologias.
Observou-se carência de estudos atualizados na literatura científica sobre dados epidemiológicos dessas crianças com MCC, com a finalidade de embasar novos estudos para qualificação do cuidado de enfermagem desses pacientes. Este estudo epidemiológico emergiu da necessidade de fundamentar um instrumento para o processo de enfermagem (PE) em UTIP, qualificando diagnósticos e intervenções de enfermagem no cuidado da criança com MCC.
Nessa perspectiva, a questão de pesquisa definida para este estudo é: “Qual é o perfil das hospitalizações de crianças menores de um ano (<1 ano) com malformações congênitas do aparelho circulatório?” Sendo assim, objetiva-se caracterizar as internações hospitalares por malformações congênitas do aparelho circulatório em crianças menores de um ano no Brasil, Rio Grande do Sul e Porto Alegre.
MÉTODOS
Trata-se de um estudo epidemiológico de série histórica e descritivo, sob as recomendações do Strengthening the Reporting of Observational Studies in Epidemiology (STROBE). Este estudo abrange dados registrados no SIH/SUS do Brasil (BR), Rio Grande do Sul (RS) e Porto Alegre (PoA) referentes às hospitalizações de <1 ano de idade com MCC, no período de 2016 a 2020. O recorte temporal da série histórica foi definido pela ausência de literatura científica atualizada sobre essa condição de saúde e cuidado para <1 ano. Os dados coletados são de domínio público disponibilizados no sítio eletrônico do DATASUS, caracterizando-se como secundários para a pesquisa. Para qualificar o perfil das hospitalizações, por conta da ausência de informação sobre nascidos vivos (NV) do ano de 2020 no DATASUS, também se coletaram dados do mesmo período e da área de abrangência da análise do Departamento de Análise de Saúde e Vigilância de Doenças Não Transmissíveis (DASTN).
A busca dos dados ocorreu no período de fevereiro a abril de 2021, na base do DATASUS denominada “epidemiológicas e morbidade”, seguida da subárea de morbidade hospitalar do SUS. As variáveis relacionadas às hospitalizações de <1 ano coletadas: local de internação por ocorrência e residência; Lista de Morbidades da Classificação Internacional das Doenças – 10ª revisão (CID-10), selecionaram-se MCC no período de janeiro de 2016 e dezembro de 2020, sexo; cor/raça; caráter de atendimento (urgência/eletiva); média de permanência; e taxa de mortalidade. No DASTN, selecionou-se o dado referente ao número de NV, considerando-se o mesmo tempo (ano). Entretanto, os dados coletados referentes aos NV no ano de 2020 são uma estimativa, pois os números oficiais ainda não haviam sido divulgados.
Os dados foram extraídos em planilhas de Excel da Microsoft®, organizados e submetidos à estatística descritiva no mesmo software, e apresentados como taxas e coeficientes em tabelas e figuras. Em se tratando de dados de domínio público, o estudo não possui aprovação do Comitê de Ética e Pesquisa; entretanto, mantém-se o respeito aos preceitos éticos com base na Resolução nº 466/2012, do Conselho Nacional de Pesquisa assim como da Lei Geral de Proteção de Dados Pessoais (LGPD), nº 13.709/2018.
RESULTADOS
Os resultados caracterizam as crianças <1 ano com MCC que foram hospitalizadas no período de 2016 a 2020 no BR por local de ocorrência e residência, totalizando 37.894 e 37.841 internações, respectivamente. No RS, houve 2.344(6,18%) e 2.301(6,08%) hospitalizações por ocorrência e residência em comparação com o total de atendimentos realizados no território brasileiro. Em POA, realizando as mesmas comparações, constataram-se 1.863(79,47%) por ocorrência e 381(16,55%) por residência.
O sexo masculino foi prevalente (52%) nas três esferas político-administrativas, considerando-se o local de ocorrência da internação. Entretanto, na análise por local de residência, o BR e RS mantêm a mesma proporção, mas em PoA, o sexo feminino assumiu a maior prevalência com 51%. Nos registros de cor/raça no BR, constatou-se que em todo o período por local de ocorrência e residência foram declarados 13.135(49,57%) como brancos, 12.392(46,76%) pardos, 652(2,46%) preta, 201(0,76%) amarela e 118(0,45%) como indígena. Observou-se a subinformação da cor/raça em 11.396(30,1%) registros por local de ocorrência e residência de <1 ano com MCC. No RS e PoA, os dados são semelhantes, respectivamente, quanto à prevalência de brancos e pardos. A Figura 1 compara o coeficiente de ocorrência e residência das internações de <1 ano com MCC por NV.
Figura 1: Coeficiente de internações hospitalares por malformações cardíacas congênitas de menores de um ano por nascidos vivos, por ocorrência e residência no Brasil, Rio Grande do Sul e Porto Alegre, 2016 a 2020.
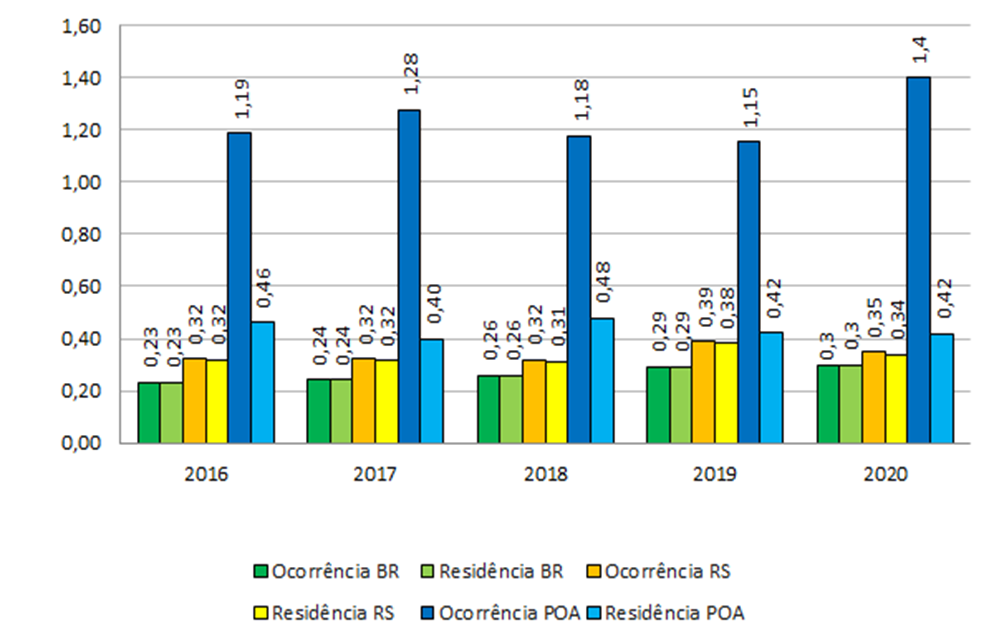
Fonte: Dados de bancos públicos do DASTN e DATASUS, Ministério da Saúde, Brasil, 2021.
O coeficiente de internações por MCC por NV no BR demonstra uma elevação de 30,4% em hospitalizações por ocorrência e residência, na comparação dos dados coletados do ano de 2016 e 2020, respectivamente. Este mesmo coeficiente do RS e PoA, representou um crescimento, ainda que menor, ao comparado ao do BR, de 9,37% e 17,64%.
Em contrapartida, cabe elucidar que o número de NV apresenta declínio desde 2018. Nos anos de 2018 e 2020, o decréscimo foi de 8,74% no BR, 6,91% e 6,81% no RS, 13,89% e 10,83% em POA, por ocorrência e residência dos NV, respectivamente. A Tabela 1 contextualiza a modalidade da hospitalização de <1 ano com MCC em caráter eletivo (agendamento) e de urgência (imediato).
Tabela 1 - Internações hospitalares por ocorrência e residência do caráter de atendimento de menores de um ano com malformações cardíacas congênitas no Brasil, Rio Grande do Sul e Porto Alegre, 2016 a 2020.
|
Modalidade de internação hospitalar |
2016 n (%) |
2017 n (%) |
2018 n (%) |
2019 n (%) |
2020 n (%) |
Total n (%) |
|
Ocorrência |
|
|
|
|
|
|
|
Eletivo (BR) |
1.648 (24,91) |
1.619 (22,90) |
1.718 (22,63) |
2.052 (24,70) |
1.761 (21,28) |
8.798 (23,24) |
|
Urgência (BR) |
4.970 (75,09) |
5.451 (77,10) |
5.874 (77,37) |
6.258 (75,30) |
6.516 (78,72) |
29.069 (76,76) |
|
Eletivo (RS) |
90 (19,65) |
78 (17,14) |
89 (19,91) |
115 (21,91) |
111 (24,18) |
483 (20,61) |
|
Urgência (RS) |
368 (80,35) |
377 (82,86) |
358 (80,09) |
410 (78,09) |
348 (75,82) |
1.861 (79,39) |
|
Eletivo (PoA) |
90 (25,06) |
77 (20,37) |
87 (24,92) |
114 (27,27) |
99 (27,57) |
467 (25,07) |
|
Urgência (PoA) |
269 (74,94) |
301 (79,63) |
262 (75,08) |
304 (72,73) |
260 (72,43) |
1.396 (74,93) |
|
Residência |
|
|
|
|
|
|
|
Eletivo (BR) |
1.648 (24,91) |
1.619 (22,90) |
1.718 (22,63) |
2.052 (24,70) |
1.761 (21,28) |
8.798 (23,24) |
|
Urgência (BR) |
4.970 (75,09) |
5.451 (77,10) |
5.874 (77,37) |
6.258 (75,30) |
6.516 (78,72) |
29.069 (76,76) |
|
Eletivo (RS) |
85 (18,76) |
72 (16,11) |
80 (18,35) |
108 (20,97) |
104 (23,11) |
449 (19,51) |
|
Urgência (RS) |
368 (81,24) |
375 (83,89) |
356 (81,65) |
407 (79,03) |
346 (76,89) |
1852 (80,49) |
|
Eletivo (PoA) |
14 (16,26) |
9 (12,16) |
15 (17,86) |
18 (25,71) |
13 (19,40) |
69 (18,10) |
|
Urgência (PoA) |
72 (83,74) |
65 (87,84) |
69 (82,14) |
52 (74,29) |
54 (80,60) |
312 (81,90) |
Fonte: Dados de bancos públicos do DATASUS, Ministério da Saúde, Brasil, 2021.
As hospitalizações possuem o caráter de urgência com a necessidade de uma assistência especializada e qualificada. No BR, observou-se a média de 76,70±1,50 hospitalizações por urgências, sendo iguais para ocorrência e residência. No RS, a média foi de 79,44±2,63 e 80,54±2,67 internações de urgência, respectivamente, por ocorrência e residência, sendo mais elevada em comparação com a do BR. Nessa ordem as hospitalizações por ocorrência e residência, a média atingiu 75,45±2,52 e 81,71±4,95 em caráter de urgência, sendo expressiva para <1 ano com MCC residentes na capital. Considerando-se o dado de 1.852 hospitalizações de urgência por residência no RS, observou-se que 1.540(83,16%) foram de crianças transferidas de outras localidades para a rede hospitalar especializada em PoA.
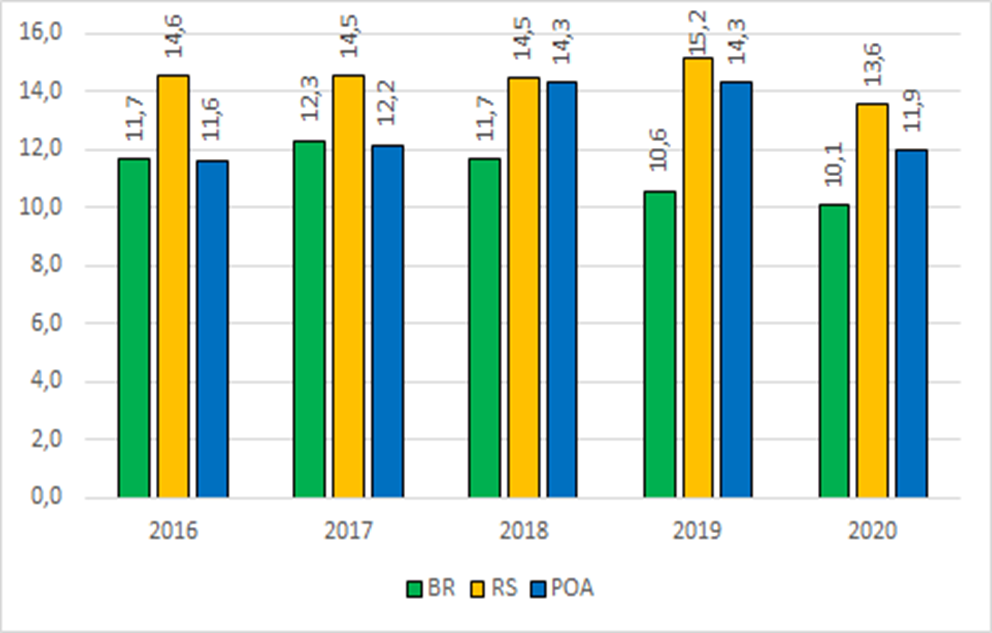
A Figura 2 expressa o tempo de permanência em dias de hospitalização por ocorrência para <1 ano com MCC avaliadas neste estudo.
Figura 2: Média de dias de permanência hospitalar por ocorrência para o diagnóstico de malformações cardíacas congênitas de menores de um ano no Brasil, Rio Grande do Sul e Porto Alegre, 2016 a 2020.
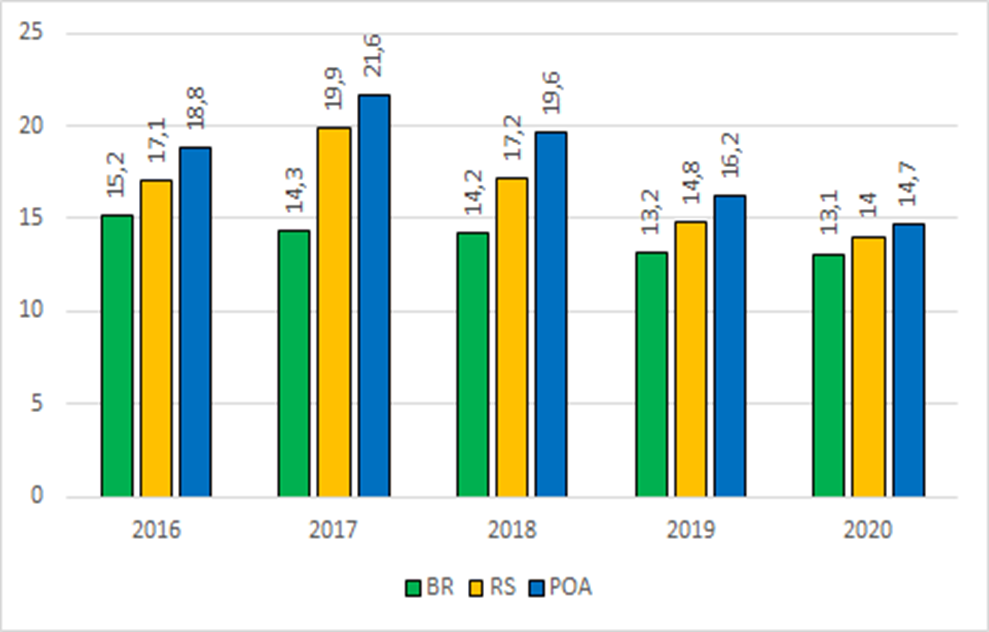
Fonte: Dados de bancos públicos do DATASUS, Ministério da Saúde, Brasil, 2021.
Na Figura 2, observou-se que a média de dias de permanência hospitalar por ocorrência de <1 ano por MCC é de em torno de 14,00±0,86 dias no BR. Verificou-se uma queda gradativa anual e, quando comparados os anos de 2016 e 2020 somente, a média de tempo de permanência hospitalar decresceu 13,82%.
O RS apresenta uma média de 16,60±2,31 dias de hospitalização; no entanto, apresenta uma redução no tempo de permanência maior ao se avaliar o mesmo período do BR (em torno de 18,12%). A média de permanência nas internações em PoA (18,18±2,74) dura em torno de dois dias a mais do que a média estadual, mas quando comparada com a média nacional, a diferença é de até cinco dias. Na comparação da média de dias de internações dos anos de 2016 e 2020, PoA tem uma redução importante de 21,8% em dias de permanência hospitalar de <1 ano por MCC. Nos anos de 2017 e 2020, RS e PoA tiveram a maior e menor média de dias de hospitalização, respectivamente. A Figura 3 apresenta a taxa de mortalidade nas hospitalizações por ocorrência de <1 ano com MCC.
Figura 3: Taxa de mortalidade hospitalar por ocorrência do diagnóstico de malformações cardíacas congênitas de menores de um ano no Brasil, Rio Grande do Sul e Porto Alegre, 2016 a 2020.
Fonte: Dados de bancos públicos do DATASUS, Ministério da Saúde, Brasil, 2021.
A Figura 3 mostra que, no BR, a taxa de mortalidade decorrente das hospitalizações por ocorrência de crianças <1 ano com MCC no período foi de 11,26±0,92 óbitos (para cada mil NV). Outro dado que se ressalta foi a redução em 14,01% dos óbitos por MCC ao se compararem o ano de 2016 e 2020. No RS, a taxa de mortalidade é de 14,45±0,68, sendo maior quando comparada à mesma taxa do BR, e tem uma menor redução de 6,93% da taxa na comparação no mesmo período. Entretanto, cabe enfatizar que no ano de 2019 ocorreu a maior taxa de mortalidade (15,15/mil NV) e, em comparação a 2020, a redução foi de 10,49%.
Na capital gaúcha, a taxa de mortalidade por ocorrência foi de 16,64±0,51 para cada mil NV com MCC. Ao se analisar a taxa do ano de 2016 e 2020, identificou-se um aumento de 2,66% da mortalidade de <1 ano com MCC, de tal modo que possíveis ações assistenciais possam não ter sido empregadas para a ocorrência de uma redução da mortalidade no período analisado.
DISCUSSÃO
Buscando o perfil epidemiológico de <1 ano com MCC e as características das hospitalizações, as informações foram colhidas a partir de dois critérios: o de residência, ou seja, pelo local onde residem essas crianças, ou o de ocorrência, quando a internação ocorre em uma localidade distinta da localidade de residência dos pacientes. No Brasil, a discrepância entre local de residência e de ocorrência das internações. Acredita-se que essa diferença está na demanda de atendimento do SUS em cidades brasileiras fronteiriças com outros países, justificando esses pacientes não residirem no local de ocorrência.
Já no nível estadual e municipal, a diferença das internações de crianças com MCC também ocorrem, sendo mais elevado em PoA, possivelmente por acolher crianças oriundas de outros municípios gaúchos. A demanda de atendimentos na capital gaúcha, emerge como centro de referência em assistência especializada para cuidados complexos realizados por profissionais com alta competência técnica na área da pediatria.(4)
Nessa perspectiva, um estudo realizado no Rio de Janeiro buscou registros de crianças <1 ano com MCC no período de 2006 a 2010: dos 345 NV com MCC, 76% dos nascimentos ocorreram em maternidades sem especialidade pediátrica ou com falta de recursos para atendimento complexo, ao passo que 54,8% desses pacientes tiveram hospitalização pós natal no Instituto Nacional de Cardiologia é um serviço de referência para MCC.(5) Prévio ao período avaliado neste estudo, uma pesquisa realizada entre janeiro e dezembro de 2015, com uma amostra de 263 pacientes submetidos à cirurgia cardíaca de correção de MCC, verificou que 93(35,4%) eram procedentes do interior do RS.(6)
Logisticamente, o RS é organizado em macrorregiões, devido ao baixo tamanho populacional da maioria dos municípios, a frequência de casos de MCC torna-se tão pequena inviabilizando centros de referência regionais. No mesmo sentido, outro estudo sobre a distribuição de leitos de UTIN no RS, verificou-se que há uma grande concentração de leitos na localidade da região metropolitana (54,6 %). As demais seis macrorregiões do RS possuem o restante dos leitos (45,4%).(7) Ainda que o RS atenda ao preconizado pelo Ministério da Saúde com 3,7 leitos/mil NV e se assemelhe ao quantitativo de leitos de UTIN dos Estados Unidos (3,37 leitos/mil NV), existe um déficit no gerenciamento de leitos para o acesso da população do interior do estado. Pressupõe-se que a realização do exame cardiofetal, ainda no pré-natal, anteciparia a identificação de MCC, para o planejamento de transferência e transporte adequado.(7)
Por conta dessa carência de acesso e pouca oferta de serviços especializados, cabe aos estados e aos municípios garantir assistência ao pré-natal na rede de Atenção Primária à Saúde (APS) com a oferta de exames de imagem, de forma a diagnosticar eventual gestação de alto-risco. Assim, a parturiente pode ser encaminhada para o centro de referência capaz de atender ao NV imediatamente após o parto.(8-9) Nos casos em que o diagnóstico de MCC se dá no momento do parto, é necessário que haja uma assistência especializada. Portanto, as equipes de transporte do recém-nascido precisam estar altamente capacitadas e ter acesso a recursos tecnológicos como monitorização com boa funcionalidade.(10)
Ao analisar o coeficiente de internações por MCC em <1 ano, por ocorrência e residência, em relação ao número de NV, observa-se uma redução desses nascimentos a partir de 2018. Contudo, no RS, houve um aumento de 6,25% de internações por residência, o que não ocorre, de acordo com os dados, em PoA, que apresenta uma redução de 8,7% dessas internações. As hospitalizações em PoA tiveram essa redução dos residentes internados, sendo possível suprir a demanda de pacientes de outras localidades, confirmada pelo crescimento dessas internações no RS já citado anteriormente.
A rede de atenção na capital concentra-se em três instituições hospitalares que recebem um número expressivo de crianças com MCC: Hospital da Criança Santo Antônio (HCSA), Hospital de Clínicas de Porto Alegre (HCPA) e Instituto de Cardiologia – Fundação Universitária de Cardiologia (IC-FUC).(11) Destaca-se o HCSA, considerado referência nacional para atendimento de alta complexidade em pediatria, que em 2019 realizou 6.582 procedimentos cirúrgicos, dos quais aproximadamente 600 foram cirurgias relacionadas à correção cirúrgica de MCC em crianças e adolescentes com idade de até 18 anos.(12) A instituição conta com um Centro de Cardiodiagnóstico e do Instituto Materno-fetal Celso Rigo (IMFCR), em uma associação entre a Santa Casa de Misericórdia de Porto Alegre e a Medicina Materno Fetal Barcelona. A união destas entidades reconhecidas mundialmente na área de Medicina e Cirurgia Fetal faz com que PoA seja referência para todo o Brasil e América Latina.(12) Complementa-se que, no ano de 2015, houve um aumento no número de leitos de UTIP no HCSA, passando de 30 para 40 leitos, o que elevou a frequência de internações em PoA, evidenciadas na Figura 1.
Existem atualmente 271 leitos de UTIP e UTIN na capital de acordo com o Cadastro Nacional de Estabelecimentos de Saúde (CNES).(13) Todavia, embora a gestão estadual e municipal deva estar devidamente organizada quanto a regulação dos leitos, existem fatores que dificultam o acesso desses usuários, tais como: o déficit de investimentos no transporte; capacitação especializada de profissionais de saúde para a assistência no deslocamento do recém-nascido ao serviço especializado; e acompanhamento integral ao pré-natal.
A instabilidade hemodinâmica do NV sugere o caráter de urgência para a hospitalização. Nesse sentido, a correção cirúrgica e a necessidade de atendimento emergencial por equipe multidisciplinar são primordiais para realizar um cuidado criterioso e ágil, especialmente, no deslocamento do recém-nascido, o que pode exigir intervenções de urgência.(8,14)
Em relação às internações por residência, os números são semelhantes nas três esferas político-administrativas em estudo. Ao analisar dados de outros estudos com hospitais pediátricos de referência, a média de permanência é semelhante à do RS. No estudo realizado no hospital público infantil de Campo Largo-Paraná, a média de permanência hospitalar de crianças foi de 16,6 dias.(1) Esse município se tornou referência na realização de procedimentos mais complexos, em que as crianças com condição clínica moderada a severa são encaminhadas para a hospitalização. No entanto, o aumento do tempo de permanência hospitalar gerado pelas possíveis complicações exige um tempo maior de acompanhamento pela equipe diante da complexidade do tratamento.(1)
O estudo realizado em UTIP de um hospital de referência em PoA, no ano de 2015, apresentou um tempo médio de permanência de 11,4 dias de internação para pacientes submetidos à cirurgia cardíaca devido à MCC.(6) Entretanto, o tempo de permanência a partir do ano de 2016 apresentou um aumento de aproximadamente seis dias na capital, corroborando os resultados do estudo do Paraná.
Em PoA, esse dado demonstra a coerência com o acréscimo de leitos de UTIP no ano de 2015 e com a melhora da assistência à criança com MCC em parceria com a IMFCR, assim como pelo incremento da tecnologia para o uso rotineiro de oxigenação por membrana extracorpórea na instituição(6), suporte esse que prolonga a hospitalização. Entretanto, acredita-se que o aumento de dias de permanência hospitalar possa ser decorrente do quantitativo de crianças <1 ano que são referenciadas para a capital e que, por diversos fatores, podem permanecer mais tempo hospitalizadas.
Segundo achados desse estudo, foi identificado um aumento da taxa de mortalidade que se eleva para 29,39% entre as crianças não residentes em PoA com MCC, mesmo com a inclusão de tecnologias aplicadas ao tratamento na capital gaúcha. Pressupõe-se que o aumento da mortalidade pode ocorrer por subdiagnóstico durante o pré-natal da MCC, pois sem a identificação de uma gestação de alto risco, a criança, ao nascimento em um hospital que não possui serviços especializados, encontra-se em uma situação desfavorável e complexa: as condições hemodinâmicas podem ser agravadas e associadas a falta de estrutura para o transporte de longas distâncias terrestres até o centro de referência, acrescida por limitações do conhecimento dos profissionais na atenção às intercorrências advindas dessas patologias ao longo do percurso.
As MCC são a terceira maior causa de morte de recém-nascidos e representam cerca de 10% das causas dos óbitos infantis, em uma proporção de 20% a 40% das mortes decorrentes de malformações.(15) Em um estudo no BR, verificou-se que 20% dos pacientes com MCC morrem antes de completar um ano de idade; contudo, devido à subnotificação, o número exato de óbitos decorrentes dessa morbidade é desconhecido.(16)
A avaliação cardiofetal no BR deve ser realizada durante a assistência de pré-natal, visto que a incidência média é de 1% de MCC, sendo superior aos dados de países com alta renda.(17) O diagnóstico precoce das MCC é de extrema importância para evitar a mortalidade neonatal mediante o tratamento apropriado ainda no pré-natal.(17) Ainda, acrescenta-se que o conhecimento prévio desta condição clínica para gestantes em localidades muito distantes de um centro de referência, oferece uma melhor margem de tempo para o serviço no município se reorganizar de forma que o parto ocorra em um ambiente com estrutura tecnológica e assistência qualificada à criança.
No BR e no RS, as taxas de mortalidade por residência dos <1 ano com MCC mostraram-se semelhantes devido à análise do macro cenário deste estudo, o que difere da situação de PoA, cujos dados apontam que as crianças <1 ano com MCC residentes em PoA têm uma sobrevida maior se comparadas às de outras localidades. Diversos fatores podem convergir para a ocorrência das vidas perdidas: ausência do pré-natal; condições limitadas e pouca disponibilidade de exames para diagnóstico precoce da MCC na APS; falta de capacitação técnica dos profissionais; falta de medicamentos capazes de tratar de forma imediata a complexidade da criança; baixa disponibilidade de leitos em UTIP no centro de referência mais próximo; condições insuficientes de deslocamento terrestre e de profissionais qualificados, de medicamentos disponíveis no trajeto, do veículo utilizado e da distância territorial a ser percorrida. Dessa forma, esses possíveis fatores merecem ser investigados para se elucidarem e se proporem estratégias que ampliem a qualidade do atendimento às crianças com MCC que chegam aos centros de referência.
De acordo com um estudo que traçou uma análise clínico-epidemiológica de pacientes com MCC no extremo norte do BR, as novas tecnologias intervencionistas, a terapia farmacológica e as novas técnicas cirúrgicas colaboraram para a redução da morbimortalidade.(18-19) Entretanto, para que de fato haja uma ampliação da sobrevida e uma redução mortalidade infantil, é preciso se pensar não somente em investir em tecnologia ou qualificação dos profissionais dos centros de referência, mas também na logística nas pequenas localidades.
As limitações deste estudo são a utilização de dados secundários provenientes da subinformação registro do formulário de autorização da internação hospitalar. Entre as variáveis, o regime de atendimento dos pacientes, como público ou privado, e a ausência da categorização da faixa etária de neonatos e lactentes são informações que, mesmo não estando disponíveis na coleta de dados, poderiam complementar os resultados.
CONCLUSÃO
Este estudo caracterizou as crianças <1 ano hospitalizadas por MCC quanto aos aspectos demográficos e as internações nas três esferas político-administrativas que geram informações relevantes para a qualificação da rede de atenção à criança. Em relação aos achados demográficos, constatou-se que PoA é o centro de referência do RS no atendimento de aproximadamente ⅘ das hospitalizações de <1 ano com MCC provenientes de outras localidades. O predomínio do sexo masculino (exceto o sexo feminino em internações por residência na capital) e cor/raça de brancos à exceção de BR, cuja proporção entre brancos e pardos é quase pareada.
O atendimento em caráter de urgência é preponderante, sendo a média de permanência em PoA superior ao comparar com a do RS e do BR (dois e cinco dias a mais, respectivamente). Todavia, a maior taxa de permanência hospitalar, assim como a taxa de mortalidade justifica-se pelos procedimentos de maior risco realizados nos hospitais porto-alegrenses. O achado importante é que a taxa de mortalidade de crianças de outros municípios eleva-se em 29,39% em comparação com a taxa das residentes na capital.
Este estudo mostrou a necessidade de os hospitais regionais se tornarem centros de referência no RS, o que pode ser alcançado por meio de investimentos em recursos tecnológicos e de educação permanente para o alcance da alta performance das equipes de saúde nas UTIP e clínico-cirúrgicas. Por fim, espera-se contribuir para a redução da taxa de mortalidade e da permanência hospitalar ao servir como base para futuras pesquisas referentes à conscientização dos profissionais da área sobre a importância dos registros de saúde para gestão dos serviços na rede de atenção à criança, à qualificação do pré-natal, a investimentos em recursos tecnológicos nos hospitais regionais, no transporte e na educação continuada de equipes de alta performance em saúde clínico-cirúrgicas e intensivistas.
Agradecimentos
Programa de Mestrados Profissionais em Enfermagem (PROFEN) do Conselho Federal de Enfermagem (COFEN) em parceria com a Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES) pelo apoio financeiro. Programa de Iniciação Científica Institucional (PIC) da Universidade Federal de Ciências da Saúde de Porto Alegre (UFCSPA) pela concessão da bolsa de iniciação científica.
REFERÊNCIAS
- Belo WA, Oselame GB, Neves EB. Clinical and hospital profile of children with congenital heart disease. Cad. saúde colet. 2016;24(2):216-220. DOI: 10.1590/1414-462X201600020258
- Magalhães SS, Chaves EMC, Queiroz MVO. Instructional design for nursing care to neonates with congenital heart defects. Texto & Contexto Enferm. 2019; 28:e20180054. DOI: 10.1590/1980-265X-TCE-2018-0054
- Melo IS, Braz P, Roquette R, Souza P, Nunes C, Dias C. Congenital heart disease prevalence in Portugal in 2015: Data from the National Register of Congenital Anomalies. Acta Med. Port. 2020;33(7-8):491-499. DOI: 10.20344/amp.12111
- 4. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Portaria Nº 210 de 15 de junho de 2004. Define Unidades de Assistência em Alta Complexidade Cardiovascular e os Centros de Referência em Alta Complexidade Cardiovascular e suas aptidões e qualidades. Diário Oficial da União (DF); 2004. [cited 2021 Jan 19]. Avaliable from: https://bvsms.saude.gov.br/bvs/saudelegis/sas/2004/prt210_15_06_2004.html
- 5. Catarino CF, Gomes MASM, Gomes SCS, Magluta C. Records of congenital heart disease in infants under one year in information systems on birth, hospitalization and death in Rio de Janeiro State, Brazil, 2006-2010. Serv. Saúde. 2017;26(3):535-543. DOI: 10.5123/S1679-49742017000300011
- 6. Rezende RQ, Ricachinevsky CP, Botta A, Angeli VR, Nogueira AJS. Assessment of PIM-2 performance among surgical patients with heart disease and correlation of results with RACHS-1. Bras. Ter. Intensiva. 2017;29(4):453-459. DOI: 10.5935/0103-507X.20170069
- 7. Alam LAA, Zucco J, Philippsen FR, Pfeifer LJ, Menezes LO. Neonatal intensive care units in Rio Grande do Sul: Distribution of beds and equity analysis. AMRIGS. 2020;64(3):348-352. Available from: https://www.amrigs.org.br/assets/images/upload/pdf/jornal/1616523805.pdf
- 8. Jesus VS, Nascimento AM, Miranda RA, Lima JS, Tyll MAG, Veríssimo AOL. Waiting for cardiac procedure in congenital heart disease: portrait of an hospital in the Amazonian Region. J. Cardiovasc. Sci. 2018;34(4):374-382. DOI: 10.5935/2359-4802.20180035
- 9. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas, Gestação de Alto Risco. Manual Técnico. 5. ed. Brasília (DF): Ministério da Saúde; 2012 [cited 2021 Mai 18]. Avaliable from: https://bvsms.saude.gov.br/bvs/publicacoes/manual_tecnico_gestacao_alto_risco.pdf
- 10. Silva BS, Bueno CKS, Bizinelli TSQ, Ribeiro ER. A segurança no transporte do paciente crítico em ambiente intra-hospitalar: uma revisão integrativa. Esp. Saúde. 2019;20(2):90-101. DOI: 10.22421/15177130-2019v20n2p90
- 11. Santa Casa de Misericórdia de Porto Alegre (SCMPA). Indicadores do Hospital da Criança Santo Antônio [Internet]. Porto Alegre: Irmandade Santa Casa de Misericórdia de Porto Alegre; 2019 [cited 2021 Jul 30]. Available from: https://www.santacasa.org.br/hospitais/hospital-da-crianca-santo-antonio/indicadores#hospital
- 12. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde. Cadastro Nacional de Estabelecimentos de Saúde [Internet]. Brasília: Departamento de Informática do Sistema Único de Saúde; 2021 [cited 2021 Jun 22]. Available from: http://cnes2.datasus.gov.br/Mod_Sumario_Municipio.asp?VEstado=43
- Pedra SRFF, Zielinsky P, Binotto CN, Martins CN, Fonseca ESVB, Guimarães ICB, et al. Diretriz brasileira de cardiologia fetal. Arq bras. cardiol. 2019;112(5):600-648. DOI: 10.5935/abc.20190075
- Saxena A, Relan J, Agarwal R, Awasthy N, Azad S, Chakrabarty M, et al. Indian guidelines for indications and timing of intervention for common congenital heart diseases: revised and updated consensus statement of the working group on management of congenital heart diseases. Ann Pediatr Cardiol. 2019;12(3):254-286. DOI: 10.4103/apc.APC_32_19
- 15. Pinto Júnior VCP, Branco KMPC, Cavalcante RC, Carvalho Junior W, Lima JRC, Freitas SM, et al. Epidemiology of congenital heart disease in Brazil. Braz J Cardiovasc Surg. 2015;30(2):219-224. DOI: 10.5935/1678-9741.20150018
- Ministério da Saúde (BR). Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Departamento de Ciência e Tecnologia. Síntese de evidências para políticas em saúde: diagnóstico precoce de cardiopatias congênitas. Brasília (DF): Ministério da Saúde; 2017 [cited 2021 Jul 18]. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/sintese_evidencias_politicas_cardiopatias_congenitas.pdf
- Soares AM. Mortalidade para cardiopatias congênitas e fatores de risco associados em recém-nascidos. um estudo de coorte. Arq. bras. cardiol. 2018;111(5):674-657. DOI: 10.5935/abc.20180203
- Siqueira AS. Cardiopatia Congênita Neonatal: Análise Clínico-epidemiológica no extremo Norte do Brasil [Dissertação]. Boa Vista (RR): Universidade Federal de Roraima; 2020 [cited 2021 Jan 12]. Available from: https://ufrr.br/procisa/index.php?option=com_phocadownload&view=category&download=1286:cardiopatias-congenitas-neonatal-analise-clinico-epidemiologica-no-extremo-norte-do-brasil-alisson-silva-siqueira-defesa-25-09-2020&id=91:dissertacoes-turma-2018&Itemid=335
- Barros APM, Freira MHS, Migoto MT. Evidências científicas dos fatores de risco para anomalias congênitas: revisão integrativa. RECOM. 2017;7:e1804. DOI: 10.19175/reco m.v7i0.1804