CHARACTERIZATION OF HOSPITALIZATIONS FOR CIRCULATORY SYSTEM CONGENITAL MALFORMATIONS APPLIANCE IN CHILDREN UNDER ONE YEAR OLD
Resumo
Objetivo: Caracterizar as internações hospitalares por malformações congênitas do aparelho circulatório em crianças menores de um ano no Brasil, Rio Grande do Sul e Porto Alegre. Método: Estudo de série histórica com informações disponibilizadas por bancos de dados de acesso públicos, no período de 2016 a 2020. Resultados: Porto Alegre é referência no atendimento das malformações congênitas, sendo ⅘ das internações provenientes de outros municípios. Predomina o atendimento em caráter de urgência. A média de permanência e a taxa de mortalidade em Porto Alegre são superiores em comparação às do estado e país, com taxa de mortalidade 29,39% maior para crianças não residentes em Porto Alegre. Conclusão: Porto Alegre tem mortalidade e permanência altas por receber casos complexos de todo o estado. É possível que investimentos em hospitais regionais, recursos tecnológicos, transporte e educação modifiquem o padrão de referência e reduzam a taxa de mortalidade e a permanência hospitalar.
DESCRITORES: Cardiopatias Congênitas; Pesquisa sobre Serviços de Saúde; Doenças e Anormalidades Congênitas, Hereditárias e Neonatais; Saúde da Criança; Indicadores de Morbimortalidade.
ABSTRACT
Objective: To characterize hospitalizations due to congenital malformations of the circulatory system in children under one year old in Brazil, Rio Grande do Sul and Porto Alegre. Method: Historical series study with information made available by publicly accessible databases, from 2016 to 2020. Results: Porto Alegre is a reference in the care of congenital malformations, with ⅘ of hospitalizations coming from other municipalities. Emergency care predominates. The average length of stay and the mortality rate in Porto Alegre are higher compared to the state and country, with a mortality rate 29.39% higher for children not residing in Porto Alegre. Conclusion: Porto Alegre has high mortality and length of stay because it receives complex cases from all over the state. It is possible that investments in regional hospitals, technological resources, transport and education will modify the reference pattern and reduce the mortality rate and hospital stay.
DESCRIPTORS: Congenital Heart Diseases; Research on Health Services; Congenital, Hereditary and Neonatal Diseases and Abnormalities; Child Health; Morbimortality Indicators.
RESUMEN
Objetivo: Caracterizar los ingresos hospitalarios por malformaciones congénitas del sistema circulatorio en niños menores de un año en Brasil, Rio Grande do Sul y Porto Alegre. Método: Estudio de series temporales con información proporcionada por bases de datos de acceso público, de 2016 a 2020. Resultados: Porto Alegre es referencia en la atención de malformaciones congénitas, con ⅘ de las hospitalizaciones provenientes de otros municipios. Predomina la atención de urgencias. La estancia media y la tasa de mortalidad en Porto Alegre son superiores a las del estado y del país, con una tasa de mortalidad 29,39% superior para los niños no residentes en Porto Alegre. Conclusión: Porto Alegre tiene alta mortalidad y estancia debido a la recepción de casos complejos de todo el estado. Es posible que inversiones en hospitales regionales, recursos tecnológicos, transporte y educación puedan cambiar el patrón de derivación y reducir la tasa de mortalidad y la estancia hospitalaria.
DESCRIPTORES: Cardiopatías Congénitas; Investigación en Servicios de Salud; Enfermedades y Anomalías Congénitas, Hereditarias y Neonatales; Salud Infantil; Indicadores de Morbilidad y Mortalidad.
INTRODUCTION
Congenital heart diseases (CHD) are cardiovascular malformations, with a high risk of death in the absence of early diagnosis and treatment. (1-2) Mostly serious, the most complex ones stand out: coarctation of the aorta, tetralogy of Fallot, hypoplastic left heart syndrome, pulmonary atresia, total anomalous pulmonary venous return, transposition of the great arteries and truncus arteriosus (3), which require specialized assistance and require a surgical approach in the newborn's first year of life (3), it is up to the specialist nurse to provide qualified and safe assistance to these children in the Pediatric Intensive Care Unit (PICU) or Neonatal Unit (NICU).
In this sense, the child with CHD will need clinical/surgical hospitalization for intervention. Records of hospitalizations in the Unified Health System (SUS) for congenital heart malformations (CHM) are available in the Hospital Information System (HIS) of the SUS managed by the Department of Informatics of the Unified Health System (DATASUS). Given these information resources, it is possible to know the epidemiological profile of SUS users, allowing the elaboration of public policies and the implementation of new technologies.
There was a lack of up-to-date studies in the scientific literature on the epidemiological data of these children with CHM, with the purpose of supporting new studies to qualify the nursing care of these patients. This epidemiological study emerged from the need to base an instrument for the nursing process (NP) in a PICU, qualifying diagnoses and nursing interventions in the care of children with CHM.
In this perspective, the research question defined for this study is: “What is the profile of hospitalizations of children younger than one year (<1 year) with congenital malformations of the circulatory system?” Therefore, the objective is to characterize hospital admissions due to congenital malformations of the circulatory system in children under one year old in Brazil, Rio Grande do Sul and Porto Alegre.
METHODS
This is an epidemiological study of historical and descriptive series, under the recommendations of Strengthening the Reporting of OBservational Studies in Epidemiology (STROBE). This study covers data registered in the SIH/SUS of Brazil (BR), Rio Grande do Sul (RS) and Porto Alegre (PoA) referring to hospitalizations of <1 year of age with CHM, from 2016 to 2020. The time frame of the historical series was defined by the absence of updated scientific literature on this health condition and care for <1 year. The collected data are in the public domain and are available on the DATASUS website, being characterized as secondary to the research. To qualify the profile of hospitalizations, due to the lack of information on live births (LB) for the year 2020 in DATASUS, data were also collected for the same period and area covered by the analysis of the Department of Health Analysis and Surveillance of Noncommunicable Diseases (DASTN - Departamento de Análise de Saúde e Vigilância de Doenças Não Transmissíveis).
The search for data took place from February to April 2021, in the DATASUS base called “epidemiological and morbidity”, followed by the SUS hospital morbidity subarea. The variables related to hospitalizations of <1 year collected: place of hospitalization by occurrence and residence; List of Morbidities of the International Classification of Diseases – 10th revision (ICD-10), CHM were selected from January 2016 to December 2020, gender; color/race; service character (urgent/elective); average length of stay; and mortality rate. In DASTN, the data referring to the number of LB was selected, considering the same time (year). However, the data collected regarding the LB in the year 2020 are an estimate, as the official numbers had not yet been released.
Data were extracted in Microsoft® Excel spreadsheets, organized and submitted to descriptive statistics in the same software, and presented as rates and coefficients in tables and figures. In the case of public domain data, the study does not have approval from the Ethics and Research Committee; however, respect for ethical precepts is maintained based on Resolution No. 466/2012, of the National Research Council, as well as the General Law for the Protection of Personal Data (LGPD - Lei Geral de Proteção de Dados Pessoais), No. 13,709/2018.
RESULTS
The results characterize children <1 year old with CHM who were hospitalized from 2016 to 2020 in BR by place of occurrence and residence, totaling 37,894 and 37,841 hospitalizations, respectively. In RS, there were 2,344(6.18%) and 2,301(6.08%) hospitalizations by occurrence and residence compared to the total number of visits performed in the Brazilian territory. In PoA, performing the same comparisons, 1,863 (79.47%) per occurrence and 381 (16.55%) per residence were found.
The male gender was prevalent (52%) in the three political-administrative spheres, considering the place of hospitalization. However, in the analysis by place of residence, BR and RS maintain the same proportion, but in PoA, females had the highest prevalence with 51%. In the records of color/race in BR, it was found that throughout the period by place of occurrence and residence, 13,135 (49.57%) were declared white, 12,392 (46.76%) brown, 652 (2.46% ) black, 201(0.76%) as yellow and 118(0.45%) as indigenous. Color/race under information was observed in 11,396 (30.1%) records by place of occurrence and residence of <1 year with CHM. In RS and PoA, the data are similar, respectively, regarding the prevalence of whites and browns. Figure 1 compares the coefficient of occurrence and residence of hospitalizations of <1 year with CHM due to LB.
Figure 1: Coefficient of hospital admissions for congenital heart malformations of children under one year of age per live births, by occurrence and residence in Brazil, Rio Grande do Sul and Porto Alegre, 2016 to 2020.
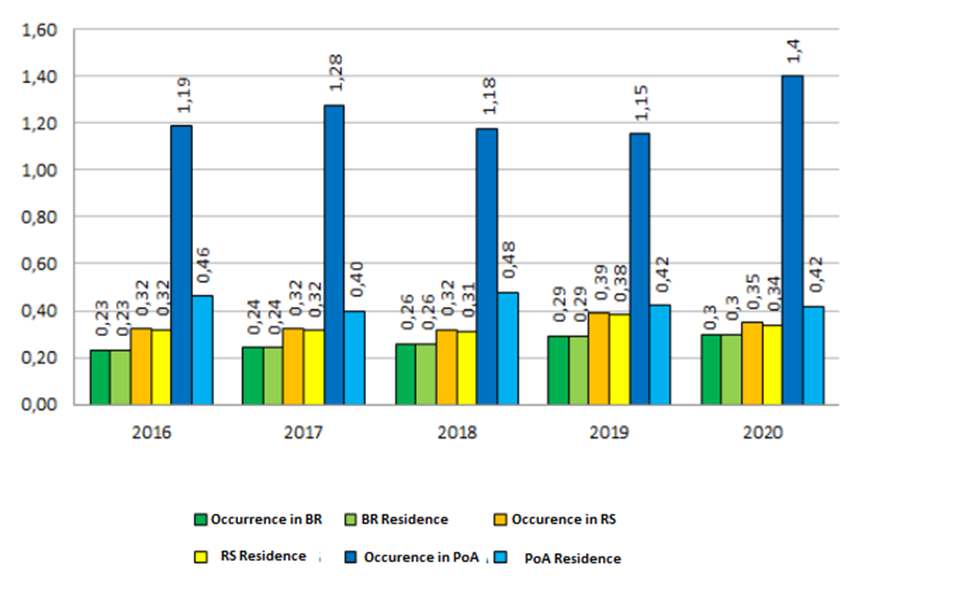
Source: Data from DASTN and DATASUS public databases, Ministry of Health, Brazil, 2021.
The coefficient of hospitalizations for CHM due to LB in BR shows a 30.4% increase in hospitalizations by occurrence and residence, when comparing data collected in 2016 and 2020, respectively. This same coefficient for RS and PoA represented growth, albeit smaller, compared to BR, of 9.37% and 17.64%.
On the other hand, it should be clarified that the number of LB has been declining since 2018. In 2018 and 2020, the decrease was 8.74% in BR, 6.91% and 6.81% in RS, 13.89% and 10.83% in POA, by occurrence and residence of LB, respectively . Table 1 contextualizes the modality of hospitalization of <1 year with CHM on an elective basis (scheduled) and urgent (immediate).
Table 1 - Hospital admissions by occurrence and residence of the nature of care for children under one year of age with congenital heart defects in Brazil, Rio Grande do Sul and Porto Alegre, 2016 to 2020.
|
Type of hospital admission |
2016 n (%) |
2017 n (%) |
2018 n (%) |
2019 n (%) |
2020 n (%) |
Total n (%) |
|
Occurrence |
|
|
|
|
|
|
|
Elective (BR) |
1.648 (24,91) |
1.619 (22,90) |
1.718 (22,63) |
2.052 (24,70) |
1.761 (21,28) |
8.798 (23,24) |
|
Urgence (BR) |
4.970 (75,09) |
5.451 (77,10) |
5.874 (77,37) |
6.258 (75,30) |
6.516 (78,72) |
29.069 (76,76) |
|
Elective (RS) |
90 (19,65) |
78 (17,14) |
89 (19,91) |
115 (21,91) |
111 (24,18) |
483 (20,61) |
|
Urgence (RS) |
368 (80,35) |
377 (82,86) |
358 (80,09) |
410 (78,09) |
348 (75,82) |
1.861 (79,39) |
|
Elective (PoA) |
90 (25,06) |
77 (20,37) |
87 (24,92) |
114 (27,27) |
99 (27,57) |
467 (25,07) |
|
Urgence (PoA) |
269 (74,94) |
301 (79,63) |
262 (75,08) |
304 (72,73) |
260 (72,43) |
1.396 (74,93) |
|
Residence |
|
|
|
|
|
|
|
Elective (BR) |
1.648 (24,91) |
1.619 (22,90) |
1.718 (22,63) |
2.052 (24,70) |
1.761 (21,28) |
8.798 (23,24) |
|
Urgence (BR) |
4.970 (75,09) |
5.451 (77,10) |
5.874 (77,37) |
6.258 (75,30) |
6.516 (78,72) |
29.069 (76,76) |
|
Elective (RS) |
85 (18,76) |
72 (16,11) |
80 (18,35) |
108 (20,97) |
104 (23,11) |
449 (19,51) |
|
Urgence (RS) |
368 (81,24) |
375 (83,89) |
356 (81,65) |
407 (79,03) |
346 (76,89) |
1852 (80,49) |
|
Elective (PoA) |
14 (16,26) |
9 (12,16) |
15 (17,86) |
18 (25,71) |
13 (19,40) |
69 (18,10) |
|
Urgence (PoA) |
72 (83,74) |
65 (87,84) |
69 (82,14) |
52 (74,29) |
54 (80,60) |
312 (81,90) |
Source: Data from DATASUS public databases, Ministry of Health, Brazil, 2021.
Hospitalizations are urgent with the need for specialized and qualified assistance. In BR, an average of 76.70±1.50 hospitalizations due to emergencies was observed, being equal for occurrence and residence. In RS, the average was 79.44±2.63 and 80.54±2.67 emergency admissions, respectively, by occurrence and residence, being higher in comparison with BR. In this order of hospitalizations by occurrence and residence, the average reached 75.45±2.52 and 81.71±4.95 in an emergency, being expressive for <1 year with CHM residing in the capital. Considering the data of 1,852 emergency hospitalizations per residence in RS, it was observed that 1,540 (83.16%) were children transferred from other locations to the hospital network specialized in PoA.
Figure 2 expresses the length of stay in days of hospitalization per occurrence for <1 year with CHM evaluated in this study.
Figure 2: Average days of hospital stay per occurrence for the diagnosis of congenital heart malformations in children under one year of age in Brazil, Rio Grande do Sul and Porto Alegre, 2016 to 2020.

Source: Data from DATASUS public databases, Ministry of Health, Brazil, 2021.
In Figure 2, it is observed that the average number of days of hospital stay per occurrence of <1 year due to CHM is around 14.00±0.86 days in the BR. There was a gradual annual decrease and, when comparing the years 2016 and 2020 alone, the average length of hospital stay decreased by 13.82%.
RS presents an average of 16.60±2.31 days of hospitalization; however, it shows a greater reduction in length of stay when evaluating the same period as the BR (around 18.12%). The mean length of stay in PoA hospitalizations (18.18±2.74) lasts around two days longer than the state average, but when compared with the national average, the difference is up to five days. Comparing the average days of hospitalization for the years 2016 and 2020, PoA has an important reduction of 21.8% in days of hospital stay of <1 year for CHM. In the years 2017 and 2020, RS and PoA had the highest and lowest average days of hospitalization, respectively. Figure 3 presents the mortality rate in hospitalizations for occurrence of <1 year with CHM.
Figura 3: Hospital mortality rate due to the diagnosis of congenital heart malformations in children under one year of age in Brazil, Rio Grande do Sul and Porto Alegre, 2016 to 2020.
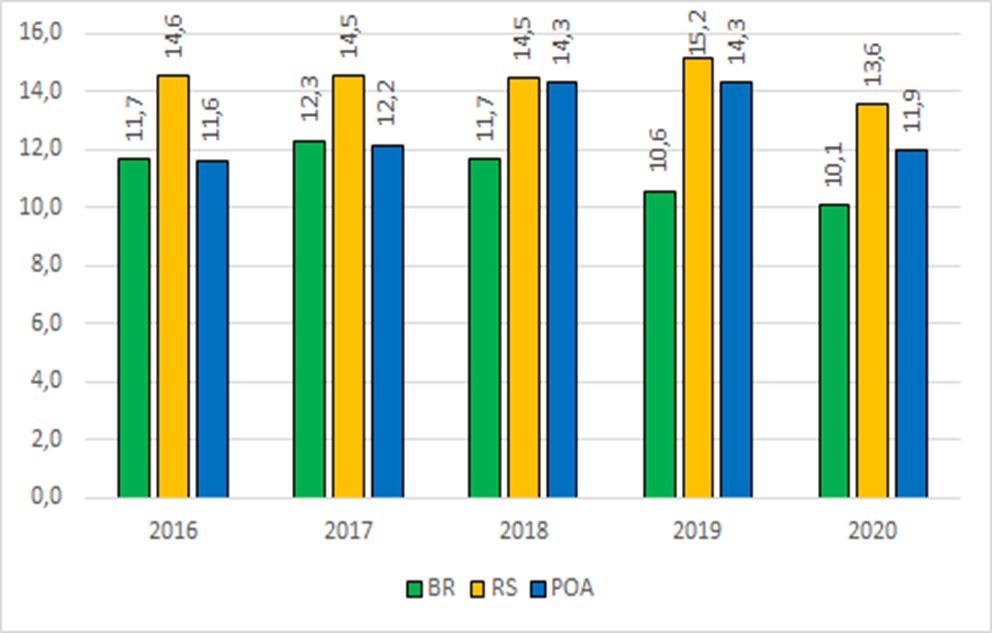
Source: Data from DATASUS public databases, Ministry of Health, Brazil, 2021.
Figure 3 shows that, in the BR, the mortality rate resulting from hospitalizations due to the occurrence of children <1 year old with CHM in the period was 11.26±0.92 deaths (for every thousand LB). Another data that stands out was the 14.01% reduction in deaths from CHM when comparing the years 2016 and 2020. In RS, the mortality rate is 14.45±0.68, which is higher when compared to the same rate in BR, and has a smaller reduction of 6.93% in the rate in the comparison in the same period. However, it should be emphasized that the highest mortality rate occurred in 2019 (15.15/thousand LB) and, compared to 2020, the reduction was 10.49%.
In the capital of Rio Grande do Sul, the mortality rate per occurrence was 16.64±0.51 for every thousand LB with CHM. When analyzing the rate for the year 2016 and 2020, a 2.66% increase in mortality of <1 year with CHM was identified, in such a way that possible care actions may not have been employed for the occurrence of a reduction in mortality in the analyzed period.
DISCUSSION
Seeking the epidemiological profile of <1 year with CHM and the characteristics of hospitalizations, information was collected based on two criteria: residence, that is, by the place where these children reside, or the occurrence, when the hospitalization takes place in a location other than the place where the patients reside. In Brazil, the discrepancy between place of residence and where hospitalizations took place. It is believed that this difference is in the demand for SUS care in Brazilian cities bordering other countries, justifying these patients not residing in the place of occurrence.
At the state and municipal level, the difference in hospitalizations of children with CHM also occurs, being higher in PoA, possibly because it accommodates children from other municipalities in Rio Grande do Sul. The demand for care in the capital of Rio Grande do Sul, emerges as a reference center in specialized assistance for complex care performed by professionals with high technical competence in the field of pediatrics.(4)
In this perspective, a study carried out in Rio de Janeiro sought records of children <1 year old with CHM in the period from 2006 to 2010: of the 345 LBs with CHM, 76% of births occurred in maternity hospitals without pediatric expertise or with a lack of resources for complex care , while 54.8% of these patients had postnatal hospitalization at the National Institute of Cardiology, which is a reference service for CHM. (5) Prior to the period evaluated in this study, a survey conducted between January and December 2015, with a sample of 263 patients undergoing cardiac surgery for CHM correction, found that 93 (35.4%) were from the interior of RS. (6)
Logistically, RS is organized into macro-regions, due to the low population size of most municipalities, the frequency of CHM cases becomes so small, making regional reference centers unfeasible. In the same sense, another study on the distribution of NICU beds in RS found that there is a large concentration of beds in the metropolitan region (54.6%). The other six macro-regions of RS have the rest of the beds (45.4%). (7) Although RS meets the recommendations of the Ministry of Health with 3.7 beds/thousand LB and is similar to the number of NICU beds in the United States (3.37 beds/thousand LB), there is a deficit in the management of beds for access by the population in the interior of the state. It is assumed that carrying out the cardiac fetal exam, still in the prenatal period, would anticipate the identification of CHM, for the transfer planning and adequate transport. (7)
Due to this lack of access and limited supply of specialized services, it is up to the states and municipalities to ensure prenatal care in the Primary Health Care (PHC) network by offering imaging tests, in order to diagnose any high-risk pregnancy. Thus, the parturient woman can be referred to the reference center capable of attending to the LB immediately after delivery. (8-9) In cases where the diagnosis of CHM occurs at the time of delivery, specialized assistance is required. Therefore, newborn transport teams need to be highly trained and have access to technological resources such as monitoring with good functionality. (10)
When analyzing the coefficient of hospitalizations for CHM in <1 year, by occurrence and residence, in relation to the number of LB, a reduction of these births is observed from 2018. However, in RS, there was an increase of 6.25% in hospitalizations per residence, which does not occur, according to the data, in PoA, which presents a reduction of 8.7% of these hospitalizations. Hospitalizations in PoA had this reduction in hospitalized residents, making it possible to meet the demand of patients from other locations, confirmed by the growth of these hospitalizations in RS, as mentioned above.
The care network in the capital is concentrated in three hospital institutions that receive a significant number of children with CHM: Hospital da Criança Santo Antônio (HCSA), Hospital de Clínicas de Porto Alegre (HCPA) and Institute of Cardiology – University Foundation of Cardiology (IC-FUC). (11) The HCSA stands out, considered a national reference for high-complexity care in pediatrics, which in 2019 performed 6,582 surgical procedures, of which approximately 600 were surgeries related to the surgical correction of CHM in children and adolescents aged up to 18 years. (12) The institution has a Cardiac Diagnosis Center and the Celso Rigo Materno-fetal Institute (IMFCR), in an association between the Santa Casa de Misericórdia de Porto Alegre and the Materno Fetal Medicine in Barcelona. The union of these entities recognized worldwide in the area of Medicine and Fetal Surgery makes PoA a reference for all of Brazil and Latin America. (12) It is complemented that, in 2015, there was an increase in the number of PICU beds at HCSA, from 30 to 40 beds, which increased the frequency of hospitalizations in PoA, shown in Figure 1.
There are currently 271 PICU and NICU beds in the capital according to the National Register of Health Establishments (CNES - Cadastro Nacional de Estabelecimentos de Saúde). (13) However, although state and municipal management must be properly organized in terms of regulating beds, there are factors that make access difficult for these users, such as: the lack of investments in transport; specialized training of health professionals to assist in the displacement of the newborn to the specialized service; and comprehensive prenatal care.
The hemodynamic instability of the LB suggests the urgency of hospitalization. In this sense, surgical correction and the need for emergency care by a multidisciplinary team are essential to provide careful and agile care, especially when moving the newborn, which may require urgent interventions. (8,14)
Regarding hospitalizations by residence, the numbers are similar in the three political-administrative spheres under study. When analyzing data from other studies with reference pediatric hospitals, the average length of stay is similar to that of RS. In the study carried out at the public children's hospital in Campo Largo-Paraná, the average hospital stay of children was 16.6 days. (1) This municipality has become a reference in performing more complex procedures, in which children with moderate to severe clinical conditions are referred for hospitalization. However, the increased length of hospital stay generated by possible complications requires a longer follow-up by the team due to the complexity of the treatment.(1)
The study carried out in the PICU of a reference hospital in PoA, in 2015, showed an average length of stay of 11.4 days of hospitalization for patients undergoing cardiac surgery due to CHM. (6) However, the length of stay from 2016 onwards increased by approximately six days in the capital, corroborating the results of the Paraná study.
In PoA, this data demonstrates consistency with the addition of PICU beds in 2015 and with the improvement of care for children with CHM in partnership with the IMFCR,
as well as the increase in technology for the routine use of extracorporeal membrane oxygenation in the institution (6), support that prolongs hospitalization. However, it is believed that the increase in days of hospital stay may be due to the number of children <1 year old who are referred to the capital and who, due to several factors, may remain hospitalized for longer.
According to the findings of this study, an increase in the mortality rate was identified, which rises to 29.39% among children who do not live in PoA with CHM, even with the inclusion of technologies applied to the treatment in the capital of Rio Grande do Sul. It is assumed that the increase in mortality may occur due to underdiagnosis during prenatal care of CHM, because without the identification of a high-risk pregnancy, the child, at birth in a hospital that does not have specialized services, finds itself in an unfavorable and complex situation: the hemodynamic conditions can be aggravated and associated with the lack of structure for transporting long distances over land to the reference center, added by limitations of the professionals' knowledge in the attention to complications arising from these pathologies along the route.
CHM are the third leading cause of death in newborns and represent about 10% of the causes of infant deaths, in a proportion of 20% to 40% of deaths resulting from malformations. (15) In a study in BR, it was found that 20% of patients with CHM die before reaching one year of age; however, due to underreporting, the exact number of deaths resulting from this morbidity is unknown. (16)
Cardiac Fetal assessment in the BR should be performed during prenatal care, as the average incidence of CHM is 1%, which is higher than data from high-income countries. (17) Early diagnosis of CHM is extremely important to prevent neonatal mortality through appropriate treatment during prenatal care. (17) Furthermore, it is added that prior knowledge of this clinical condition for pregnant women in locations very far from a reference center, offers a better margin of time for the service in the municipality to reorganize itself so that the birth takes place in an environment with technological structure and qualified assistance to the child.
In BR and RS, mortality rates per residence of <1 year olds with CHM were similar due to the analysis of the macro scenario of this study, which differs from the PoA situation, whose data indicate that children <1 year old with CHM residing in PoA have a longer survival compared to those from other locations. Several factors can converge to the occurrence of lost lives: lack of prenatal care; limited conditions and little availability of exams for early diagnosis of CHM in PHC; lack of technical training of professionals; lack of medication capable of immediately treating the child's complexity; low availability of PICU beds at the nearest referral center; insufficient conditions for land travel and qualified professionals, medicines available on the way, the vehicle used and the territorial distance to be covered. Thus, these possible factors deserve to be investigated in order to elucidate and propose strategies that increase the quality of care for children with CHM who arrive at reference centers.
According to a study that outlined a clinical-epidemiological analysis of patients with CHM in the far north of BR, new interventional technologies, pharmacological therapy and new surgical techniques collaborated to reduce morbidity and mortality. (18-19) However, for an increase in survival and a reduction in infant mortality, it is necessary to think not only about investing in technology or training of professionals in reference centers, but also in logistics in small locations.
The limitations of this study are the use of secondary data from the sub-information on the hospitalization authorization form. Among the variables, the patient care regime, such as public or private, and the absence of categorization of the age range of neonates and infants are information that, even though not available in data collection, could complement the results.
CONCLUSION
This study characterized children <1 year old hospitalized for CHM in terms of demographics and hospitalizations in the three political-administrative spheres that generate relevant information for the qualification of the child care network. Regarding the demographic findings, it was found that PoA is the RS reference center in the care of approximately ⅘ of hospitalizations of <1 year with CHM from other locations. The predominance of males (except for females in hospitalizations due to residence in the capital) and color/race of whites, with the exception of BR, whose proportion between whites and browns is almost even.
Urgent care is predominant, with the average stay in PoA being higher when compared to RS and BR (two and five days longer, respectively). However, the higher hospital stay rate, as well as the mortality rate, is justified by the higher risk procedures performed in hospitals in Porto Alegre. The important finding is that the mortality rate of children from other municipalities increases by 29.39% compared to the rate of residents in the capital.
This study showed the need for regional hospitals to become reference centers in RS, which can be achieved through investments in technological resources and continuing education to achieve high performance of health teams in PICUs and clinical-surgical units. Finally, it is expected to contribute to the reduction of the mortality rate and hospital stay by serving as a basis for future research regarding the awareness of professionals in the area about the importance of health records for the management of services in the child care network, prenatal qualification, investments in technological resources in regional hospitals, transportation and continuing education of high-performance teams in clinical-surgical health and intensivists.
Acknowledgements
Professional Master's Program in Nursing (PROFEN) of the Federal Council of Nursing (COFEN) in partnership with the Coordination for the Improvement of Higher Education Personnel (CAPES) for financial support. Institutional Scientific Initiation Program (PIC) of the Federal University of Health Sciences of Porto Alegre (UFCSPA) for granting the scientific initiation scholarship.
REFERÊNCIAS
-
- Belo WA, Oselame GB, Neves EB. Clinical and hospital profile of children with congenital heart disease. Cad. saúde colet. 2016;24(2):216-220. DOI: 10.1590/1414-462X201600020258
- Magalhães SS, Chaves EMC, Queiroz MVO. Instructional design for nursing care to neonates with congenital heart defects. Texto & Contexto Enferm. 2019; 28:e20180054. DOI: 10.1590/1980-265X-TCE-2018-0054
- Melo IS, Braz P, Roquette R, Souza P, Nunes C, Dias C. Congenital heart disease prevalence in Portugal in 2015: Data from the National Register of Congenital Anomalies. Acta Med. Port. 2020;33(7-8):491-499. DOI: 10.20344/amp.12111
- 4. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Portaria Nº 210 de 15 de junho de 2004. Define Unidades de Assistência em Alta Complexidade Cardiovascular e os Centros de Referência em Alta Complexidade Cardiovascular e suas aptidões e qualidades. Diário Oficial da União (DF); 2004. [cited 2021 Jan 19]. Avaliable from: https://bvsms.saude.gov.br/bvs/saudelegis/sas/2004/prt210_15_06_2004.html
- 5. Catarino CF, Gomes MASM, Gomes SCS, Magluta C. Records of congenital heart disease in infants under one year in information systems on birth, hospitalization and death in Rio de Janeiro State, Brazil, 2006-2010. Serv. Saúde. 2017;26(3):535-543. DOI: 10.5123/S1679-49742017000300011
- 6. Rezende RQ, Ricachinevsky CP, Botta A, Angeli VR, Nogueira AJS. Assessment of PIM-2 performance among surgical patients with heart disease and correlation of results with RACHS-1. Bras. Ter. Intensiva. 2017;29(4):453-459. DOI: 10.5935/0103-507X.20170069
- 7. Alam LAA, Zucco J, Philippsen FR, Pfeifer LJ, Menezes LO. Neonatal intensive care units in Rio Grande do Sul: Distribution of beds and equity analysis. AMRIGS. 2020;64(3):348-352. Available from: https://www.amrigs.org.br/assets/images/upload/pdf/jornal/1616523805.pdf
- 8. Jesus VS, Nascimento AM, Miranda RA, Lima JS, Tyll MAG, Veríssimo AOL. Waiting for cardiac procedure in congenital heart disease: portrait of an hospital in the Amazonian Region. J. Cardiovasc. Sci. 2018;34(4):374-382. DOI: 10.5935/2359-4802.20180035
- 9. Ministério da Saúde (BR). Secretaria de Atenção à Saúde. Departamento de Ações Programáticas Estratégicas, Gestação de Alto Risco. Manual Técnico. 5. ed. Brasília (DF): Ministério da Saúde; 2012 [cited 2021 Mai 18]. Avaliable from: https://bvsms.saude.gov.br/bvs/publicacoes/manual_tecnico_gestacao_alto_risco.pdf
- 10. Silva BS, Bueno CKS, Bizinelli TSQ, Ribeiro ER. A segurança no transporte do paciente crítico em ambiente intra-hospitalar: uma revisão integrativa. Esp. Saúde. 2019;20(2):90-101. DOI: 10.22421/15177130-2019v20n2p90
- 11. Santa Casa de Misericórdia de Porto Alegre (SCMPA). Indicadores do Hospital da Criança Santo Antônio [Internet]. Porto Alegre: Irmandade Santa Casa de Misericórdia de Porto Alegre; 2019 [cited 2021 Jul 30]. Available from: https://www.santacasa.org.br/hospitais/hospital-da-crianca-santo-antonio/indicadores#hospital
- 12. Ministério da Saúde (BR). Departamento de Informática do Sistema Único de Saúde. Cadastro Nacional de Estabelecimentos de Saúde [Internet]. Brasília: Departamento de Informática do Sistema Único de Saúde; 2021 [cited 2021 Jun 22]. Available from: http://cnes2.datasus.gov.br/Mod_Sumario_Municipio.asp?VEstado=43
- Pedra SRFF, Zielinsky P, Binotto CN, Martins CN, Fonseca ESVB, Guimarães ICB, et al. Diretriz brasileira de cardiologia fetal. Arq bras. cardiol. 2019;112(5):600-648. DOI: 10.5935/abc.20190075
- Saxena A, Relan J, Agarwal R, Awasthy N, Azad S, Chakrabarty M, et al. Indian guidelines for indications and timing of intervention for common congenital heart diseases: revised and updated consensus statement of the working group on management of congenital heart diseases. Ann Pediatr Cardiol. 2019;12(3):254-286. DOI: 10.4103/apc.APC_32_19
- 15. Pinto Júnior VCP, Branco KMPC, Cavalcante RC, Carvalho Junior W, Lima JRC, Freitas SM, et al. Epidemiology of congenital heart disease in Brazil. Braz J Cardiovasc Surg. 2015;30(2):219-224. DOI: 10.5935/1678-9741.20150018
- Ministério da Saúde (BR). Secretaria de Ciência, Tecnologia e Insumos Estratégicos. Departamento de Ciência e Tecnologia. Síntese de evidências para políticas em saúde: diagnóstico precoce de cardiopatias congênitas. Brasília (DF): Ministério da Saúde; 2017 [cited 2021 Jul 18]. Available from: https://bvsms.saude.gov.br/bvs/publicacoes/sintese_evidencias_politicas_cardiopatias_congenitas.pdf
- Soares AM. Mortalidade para cardiopatias congênitas e fatores de risco associados em recém-nascidos. um estudo de coorte. Arq. bras. cardiol. 2018;111(5):674-657. DOI: 10.5935/abc.20180203
- Siqueira AS. Cardiopatia Congênita Neonatal: Análise Clínico-epidemiológica no extremo Norte do Brasil [Dissertação]. Boa Vista (RR): Universidade Federal de Roraima; 2020 [cited 2021 Jan 12]. Available from: https://ufrr.br/procisa/index.php?option=com_phocadownload&view=category&download=1286:cardiopatias-congenitas-neonatal-analise-clinico-epidemiologica-no-extremo-norte-do-brasil-alisson-silva-siqueira-defesa-25-09-2020&id=91:dissertacoes-turma-2018&Itemid=335
- Barros APM, Freira MHS, Migoto MT. Evidências científicas dos fatores de risco para anomalias congênitas: revisão integrativa. RECOM. 2017;7:e1804. DOI: 10.19175/reco m.v7i0.1804






