EFFECT OF THE ELMO HELMET AS A MEASURE TO REDUCE INTUBATION IN TIMES OF COVID 19
RESUMO
Objetivo: Avaliar os efeitos do capacete ELMO como medida de redução da necessidade de intubação em pacientes hospitalizados com COVID-19. Método: Trata-se de uma pesquisa de caráter prospectivo, quantitativo e descritivo com uma amostragem. A coleta de dados ocorreu entre maio e junho de 2021, com 28 pacientes com COVID-19 e divididos em dois grupos: Grupo Tratamento Convencional e Grupo Capacete ELMO cpap. Resultados: Quanto à intubação, 10 (30%) foram intubados após sessão ELMO cpap, o SOFA foi de 243 (7,4%), e 6 (18%) evoluíram à óbito. Para pacientes entubados, 46% foram evidenciados no GCE e 30% no GTC. Ainda, quanto ao desfecho 32% do GCE e 6% do GTC evoluíram para óbito. Conclusão: Diante deste contexto, constata-se que o Elmo Cpap não se mostrou vantajoso em relação ao tratamento convencional; e, o aumento das pequenas sessões de fisioterapia respiratória indica uma melhora na evolução clínica da doença.
DESCRITORES: Pneumonia; SARS-CoV-2; COVID-19; Dispositivos de proteção respiratória; Pressão positiva contínua nas vias aéreas; Ventilação não invasiva.
ABSTRACT
Objective: To evaluate the effects of the ELMO helmet as a measure to reduce the need for intubation in patients hospitalized with COVID-19. Method: This is a prospective, quantitative and descriptive study with a sample. Data collection took place between May and June 2021, with 28 patients with COVID-19 and divided into two groups: Conventional Treatment Group and Helmet ELMO cpap Group. Results: As for intubation, 10 (30%) were intubated after an ELMO cpap session, the SOFA was 243 (7.4%), and 6 (18%) died. For intubated patients, 46% were evidenced in the EHG and 30% in the CTG. Still, regarding the outcome, 32% of the EHG and 6% of the CTG evolved to death. Conclusion: Given this context, it appears that Elmo Cpap did not prove to be advantageous compared to conventional treatment; and, the increase in small sessions of respiratory physiotherapy indicates an improvement in the clinical evolution of the disease.
DESCRIPTORS: Pneumonia; SARS-CoV-2; COVID-19; Respiratory protection devices; Continuous positive airway pressure; Non-invasive ventilation.
RESUMEN
Objetivo: Evaluar los efectos del casco ELMO como medida para reducir la necesidad de intubación en pacientes hospitalizados con COVID-19. Método: Se trata de una investigación prospectiva, cuantitativa y descriptiva con una muestra. La recogida de datos se realizó entre mayo y junio de 2021, con 28 pacientes con COVID-19 y divididos en dos grupos: Grupo Tratamiento Convencional y Grupo Casco ELMO cpap. Resultados: En cuanto a la intubación, 10 (30%) fueron intubados después de la sesión de ELMO cpap, el SOFA fue de 243 (7,4%), y 6 (18%) evolucionaron a muerte. En el caso de los pacientes intubados, el 46% se evidenció en el GCE y el 30% en el GTC. Asimismo, respecto al desenlace el 32% de los GCE y el 6% de los GTC evolucionaron a muerte. Conclusión: En este contexto, se constató que Elmo Cpap no fue ventajoso sobre el tratamiento convencional; y, el aumento de pequeñas sesiones de fisioterapia respiratoria indica una mejoría en la evolución clínica de la enfermedad.
DESCRIPTORES: Neumonía; SARS-CoV-2; COVID-19; Dispositivos de protección respiratoria; Presión positiva continua en la vía aérea; Ventilación no invasiva.
INTRODUCTION
The early use of non-invasive ventilation (NIMV) in patients with viral infection has gained importance in the treatment of severe acute respiratory syndrome, resulting in a higher success rate, reduction in mortality rates, endotracheal intubation, and related complications in patients with acute respiratory infection. 1,2
What determines the success of non-invasive mechanical ventilation (NIMV) is the selection of the interface, as there are a variety of interfaces available (nasal, facial, oronasal, full facial, nasal pillows and helmet). 3 Addressing the characteristics and performance of the different interfaces helps in selecting the most appropriate one for the patient, increasing the probability of NIMV success. 4
The total facial interface and the helmet have the advantages of reducing air output and the possibility of using higher values for inspiratory pressures, since there is a greater area of contact between this interface and the patient's face. In addition, the interfaces reduce the risk of skin damage, which makes them more comfortable. 5
The helmet is the interface that can help improve comfort during non-invasive ventilation (NIV), the strategy eliminates the need for a seal around the nose and mouth. In prospective non-randomized studies comparing the use of a helmet interface and a face mask, a reduction in the rate of intubation related to intolerance was observed, allowing continuous delivery of NIV for longer periods. 6
Brazil is experiencing difficulties, lack of mechanical ventilators, and in view of this, it was imagined that there would be a shortage of these machines to treat patients as was happening in other countries, such as Italy for example. In the state of Maranhão, the collapse of the Intensive Care Units (ICU) was announced, and this scenario was also present throughout Brazil. This concern thus justifies research by being an intensivist physician together with research hospitals to find solutions and validate the various alternatives suggested and used in the most diverse ways.
In Brazil, the idea was presented by the superintendent of ESP/CE, Dr. Marcelo Alcântara, known as ELMO, who comes with the promise to relieve ICUs, which are already saturated with patients with COVID-19. And thinking about this possibility, we emphasize the use of ELMO in 13 patients with COVID-19 who were randomly assigned to NIV applied through an ELMO helmet versus standard protocol of other devices (O2 catheter, high-flow cannula, face mask ), or not use, according to clinical staff protocols.
The current research was preceded by a study carried out by Holanda (2021), where he states that the helmet is conceived as something non-invasive, which can prevent intubation in up to 60% of patients, offering a lower risk of viral dispersion, as the helmet seals 100% around the patient's face, which he can cough into, without releasing viral particles into the environment, allowing positive pressure, and without the need for electrical energy. The aforementioned author states that due to the demand of patients in ICUs, the device can also be applied in apartments or wards.
Given this context, the question is: What are the best evidence and recommendations for the use of ELMO to reduce intubation in patients with Covid 19?
The cost and logistics of acquiring mechanical ventilation equipment can end up being an obstacle in the management of emergency health services, and consequently making its practice unfeasible in inserted health systems, lacking urgent financial resources, which stimulates the need for more viable alternatives of non-invasive ventilation with ELMO among patients with ARF.
The objective of the research was to evaluate the effects of the ELMO helmet as a measure to reduce the need for intubation in patients hospitalized with COVID-19.
METHODS
The research was prospective, quantitative and descriptive with intentional sampling. This research procedure aims to seek frequency, distinction, relationship and association between variables, record experiences, observations, unusual events. Performed in patients under treatment in a reference unit for the treatment of COVID-19.
The research was conducted in a health care center, the Hospital das Clínicas Integradas (HCI), located in the city of São Luís, Maranhão, referenced by the Government of the State of Maranhão in the first half of 2020 for exclusive assistance to patients with Coronavirus (COVID-19 and SARS-CoV-2) and acute respiratory syndromes.
In a follow-up way, 61 patients with Covid 19 were included, regardless of age or gender. Patient records will be acquired from a single treatment center located in the State of Maranhão. It was divided into two comparison groups. The first group consisted of 33 patients randomized to the group without intervention using the ELMO, and using the institution's standard protocol, and using a nasal catheter, mask, the attempt at NIV with other devices such as oro-nasal masks, and the second group with 28 patients who used ELMO, to verify the rate of tracheal intubation, and improvement of gasometric parameters, lactate, and hospital mortality.
For the inclusion criteria, it was part: Patient alert, cooperative; Use of oxygen therapy with nasal oxygen catheter ≥ 4L/min or mask with reservoir ≥ 8 L/min maintaining SpO2 > 92%; presenting f > 25μpm; Gasometric parameters (pre-ELMO cpap) pH> 7.35, PaO2>70 mmHg, PaO2/ FIO2<250 and Chest X-ray or CT scan with bilateral parenchymal capacity in the last 24 hours. The variables that were evaluated were: age, gender, degree of impairment in the chest imaging exam (chest tomography), positive PCR test (COVID -19), arterial blood gases (requested when there are breathing problems).
As for exclusion, the recommendations guided by Schettino et al.9, who pointed out the following contraindications for the use of non-invasive ventilation with positive pressure, such as: decreased consciousness, drowsiness, agitation, confusion or patient refusal; hemodynamic instability requiring vasopressor medication, shock (systolic blood pressure < 90 mmHg), complex arrhythmias; upper airway obstruction or facial trauma; ineffective coughing or inability to swallow; abdominal distention, nausea or vomiting; upper digestive bleeding; acute myocardial infarction; recent postoperative period of facial, upper airway or esophageal surgery; use of non-invasive ventilation (NIV) which is controversial; postoperative period of gastric surgery and pregnancy.
Among the primary outcomes that were evaluated, there are: hospital mortality, intubation rate and complications. Secondary outcomes included: need for invasive mechanical ventilation (IMV), time on IMV, need for intensive care unit (ICU), length of stay in the ICU, arterial blood gas exchange [pH, ratio between partial pressure of arterial oxygen and fractional inspired oxygen (PaO2 / FiO2) and partial pressure of blood carbon dioxide (PaCO2)], respiratory rate and other vital signs (heart rate, blood pressure, among others), use of vasopressor drugs, SOFA scale or equivalent (PATEL et al., 2016; GÜRBÜZ et al., 2015).
There were two groups: Conventional Treatment Group (CTG) – patients who received treatment according to the pre-established protocol by the State Department of Health (SES - Secretaria de Estado da Saúde) of the Maranhão State government and ELMOcpap Helmet Group (EHG), which includes: low cost and association of non-invasive ventilation with orofacial oxygen mask in the patient. Patient data will be paired at equal serial time intervals according to the most frequent checks in the medical records from admission to discharge. 10
These patients were invited to participate in the research, where they were informed and instructed about the device they would use. All doubts were removed regarding the proposed intervention. After all the information, the intervention only started after the patient fully understood the protocol and signed the Free and Informed Consent Form (FICF).
After inclusion, the preparation phase began with the positioning of the patient on the bed in the Fowler position, semi-sitting at 45º and instructed to remove any accessory and dental prostheses, put on a cap and ear protectors before placing the ELMOcpap. A multiparametric monitor was installed for continuous monitoring of cardiorespiratory variables: peripheral oxygen saturation (SpO2), heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), mean arterial pressure (MAP). The rebreathing of carbon dioxide was evaluated in the first application of ELMOcpap by capnography with measurement of the inspired pressure of carbon dioxide (CO2) to titrate the total flow of gases and avoid risks of CO2 rebreathing.
The ELMOcpap was placed on the patient by previously trained professionals. The CPAP level was adjusted by a springload PEEP valve at 8cm H2O initially, with an increase of 2 cm H2O every 2 minutes according to the patient's needs, not exceeding 12 cm H2O to avoid adverse effects. 12 To measure CPAP, an analog cuff meter was adapted, connected to the adapter next to the HEPA filter at the air outlet.
The full flow supply of oxygen (O2) and compressed air has been accommodated to provide 60 L/min initially 13,14 and an initial FIO2 titrated to a target SpO2>94% calculated by the formula. 15
FIO2=(AC flow x 0.21+02 flow x 1.00)/(Total flow x 100)
The clinical and demographic characteristics of the patients were collected by a single duly trained collaborator: age, sex, Sequential Organ Failure Assessment (SOFA) - considered the gold standard in the diagnosis of sepsis, and should not be used for patient management, blood gas analysis after hospital admission. For patients who were part of the Capacete ELMOcpap Group, the total number of sessions, duration of hospital stay, orotracheal intubation after the ELMO session, adverse effects and the result of using ELMOcpap were used. The following outcomes were described: use of invasive mechanical ventilation, discharge or death.
The tabulation and statistical analysis of the data was made in the Excel 2010 program. For this purpose, the results were presented in the form of graphs and tables, descriptively analyzed using mean, standard deviation and median, statistically significant were considered when the alpha was less than 5%. The normality test was preceded by Shapiro-Wilk and Kolmogorov-Smirnov, comparisons were made throughout the follow-up by test and student or its non-parametric counterpart (Mann-Whitney), and other comparisons by Wilcoxon, ANOVA (or its non-parametric counterpart: Kruskal-Wallis).
The study was approved by the National Research Ethics Committee (CONEP - Comissão Nacional de Ética em Pesquisa) and is in accordance with resolution 466/2012 of the National Health Council (CNS - Conselho Nacional de Saúde). 16 All patients signed the Informed Consent Form (ICF) to participate in the study, having the right to anonymity, secrecy and confidentiality of the information obtained, as well as the freedom to refuse to participate in the proposed activities and questions.
RESULTS
In order to evaluate the patients, it was necessary to carry out a panorama, where when starting the visits to the patients, they were observed at the bedside, before including the patients for the research. Of these, 61 patients diagnosed with moderate to severe COVID-19 met the eligibility criteria, with 33 not using ELMOcpap and 28 patients undergoing the protocol and application of ELMOcpap.
Demographic and clinical characteristics are shown in Table 1, 36% of participants in the ELMOcpap Helmet Group (EHG) were elderly, two participants in the same group were 106 and 108 years old, 64% were men and 50% between 11 and 30 days of hospitalization. In the Conventional Treatment Group (CTG), there were similar values of 24% for ages 40 to 49 years and 60 to 69 years, consecutively, women prevailed in this group with 52% and 48% between 11 and 30 days of hospitalization.
Table 1. Demographic and clinical characteristics of patients
|
|
EHG |
CTG |
||
|
|
n° |
p |
n° |
p |
|
Age |
|
|
|
|
|
20 to 59 years |
11 |
39,29% |
20 |
60,61% |
|
> 60 years |
17 |
60,71% |
13 |
39,39% |
|
|
|
|
|
|
|
Gender |
|
|
|
|
|
Female |
10 |
35,71% |
17 |
51,52% |
|
Male |
18 |
64,29% |
16 |
48,48% |
|
Hospitalization days |
|
|
|
|
|
<5 days |
3 |
11% |
1 |
3% |
|
5 to 10 days |
8 |
29% |
13 |
39% |
|
11 to 30 days |
14 |
50% |
16 |
48% |
|
> 30 days |
3 |
11% |
3 |
9% |
|
Σ |
28 |
100% |
33 |
100% |
Source: own authorship, 2022.
Regarding the outcome, for a better understanding of what is presented in the calculations, it is clear that the ELMO was not effective in relation to mortality in relation to the EHG (33%) in terms of patients not treated with an ELMO helmet (18%), in the ICU and/or being placed on mechanical ventilation.
Severity on admission was determined by the score obtained on the SOFA (Sequential Organ Failure Assessment), which is a measurement parameter to analyze the health conditions of critically ill patients, including their chances of survival. Graph 1, shows the score obtained in the SOFA between severe (22 [43%] of the EHG and 29 [57%] of the CTG) and extremely severe (6 [60%] of the EHG and 4 [40%] of the CTG), and 04 patients from the EHG evolved to death (demonstrated in Graph 1).
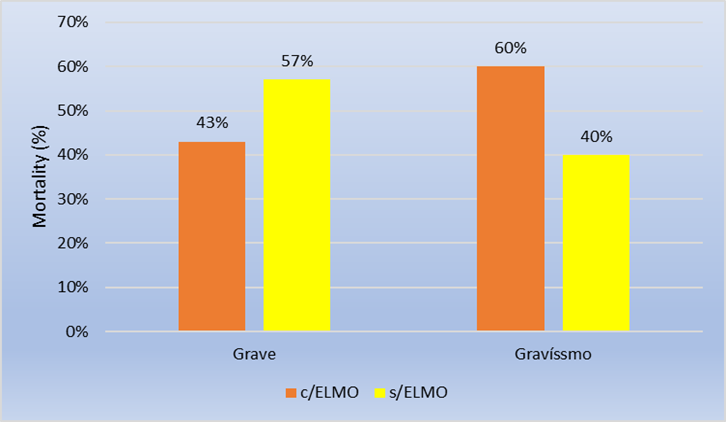
Graph 1. Demonstration of the score obtained in the SOFA
Source: own authorship, 2022.
As for the score obtained from PaO2/FIO2, it was shown that 13 (46%) of the patients participating in the EHG were scored as severe ≤ 100 mmHg (demonstrated in graph 2).
The absolute values of the PaO2/FIO2 parameters are shown in Graph 2.
Graph 2. Parameters of the score obtained in PaO2/FIO2
Source: own authorship, 2022.
Regarding arterial blood gas parameters and cardiorespiratory parameters, two groups of the CEG were divided, patients with even numbers and patients with odd numbers, during the first hour of an ELMOcpap session. Patients 8 and 13 were excluded because the parameters were not included, leading to withdrawals for this analysis.
The average result of the blood gas tests, according to Table 2, showed an increase in PO2 in 1 hour (139.95) after the session with a decrease after 6-12 hours (113.01).
Table 2. Arterial blood gas parameters before the first session of ELMOcpap, 1 hour after and 6-12 hours in individual patients (P1-P28). *p<0.05
|
Characteristics |
Before |
1h After |
6-12h After |
|
pH |
7,44 |
7,43 |
7,41 |
|
PaCO2 |
34,35 |
34,91 |
34,4 |
|
PO2 |
88,75 |
139,95 |
113,01 |
|
HCO2 |
26,39 |
24,59 |
23,4 |
|
Lactate |
1,56 |
1,42 |
1,18 |
Source: own authorship, 2022.
The adverse effects observed with the EHG were scored in length of hospital stay, 11 (39%) were hospitalized between 1 to 5 days. As for intubation, 13 (46%) were intubated after the ELMOcpap session, the SOFA was 229 (8.2%), and 9 (32%) died. In the CTG, length of hospital stay was scored, 21 (64%) were hospitalized between 6 and 14 days. As for intubation, 10 (30%) were intubated after the ELMOcpap session, the SOFA was 243 (7.4%), and 6 (18%) died (Table 3).
Table 3. Factors associated with the response to the use of ELMO cpap and the Conventional Treatment group
|
Characteristics |
EHG |
CTG |
||||||||||||
|
|
|
|
||||||||||||
|
Length of hospital stay |
|
|
|
|
|
|||||||||
|
1-5 days |
11 |
39% |
2 |
6% |
|
|||||||||
|
6-14 days |
10 |
36% |
21 |
64% |
|
|||||||||
|
15-30 days |
4 |
14% |
8 |
24% |
|
|||||||||
|
>30 days |
3 |
11% |
2 |
6% |
|
|||||||||
|
Orotracheal intubation after ELMO cpap session |
|
|
|
|||||||||||
|
Yes |
13 |
46% |
10 |
30% |
|
|||||||||
|
No |
15 |
54% |
23 |
70% |
|
|||||||||
|
SOFA |
229 |
8,2% |
243 |
7,4% |
|
|||||||||
|
Outcome |
|
|
|
|
|
|||||||||
|
Hospital discharge |
19 |
68% |
27 |
82% |
|
|||||||||
|
Death |
9 |
32% |
6 |
18% |
|
|||||||||
|
Σ |
28 |
100% |
33 |
100% |
|
|||||||||
Source: own authorship, 2022.
DISCUSSION
In the current study, 61 patients were observed, called EHG and CTG, which showed the use of ELMO, a helmet-like device capable of offering CPAP, through continuous flow of oxygen and compressed air for patients with respiratory failure due to COVID-19 who required O2 supplementation. The population groups that are most affected by Covid-19 are aged 60 years or older and individuals diagnosed with chronic diseases. 17
Search carried out by Porto 18 shows that mortality rates increase gradually according to age, that is, people aged 40 years. The rate in Brazil is 0.4%; 50 years is 1.3%; 60 years is 3.6%; 70 years old, the rate rises to 8%, and over 80 years old, it rises to 14.8%. 18 Data from China indicate that older adults, individually those with serious underlying health conditions, are at higher risk of death from Covid-19. 19 Although most cases of Covid-19 reported in China were mild (81%), approximately 80% of deaths occurred among adults aged ≥60 years; only one (0.1%) death occurred in a person aged ≤19 years. 20 This happens due to underlying conditions such as hypertension, diabetes, chronic cardiovascular and respiratory diseases, and cancer. 21
The discriminant accuracy of the SOFA score for predicting mortality in patients before intubation for COVID-19 pneumonia was poor and significantly lower than using age alone. This finding has several potential explanations. 23 The SOFA score was designed for patients with sepsis and only 3 of 6 equally weighted organ system surrogates (respiratory, renal, and hepatobiliary) are associated with mortality in COVID-19. 24, 25,26 In the current survey, 10 patients in the CTG and 13 in the EHG had respiratory failure requiring mechanical ventilation, which is the leading cause of death in patients with COVID-19.
The success rate described in the current research corroborates Tomaz's research 27, however, there was a significant improvement in oxygenation after ELMOcpap sessions of 30-60 min, while in the current research it was observed only after 6-12h. In another retrospective observational cohort study 28 which involved 306 patients, which showed that treatment with 10 cmH2O CPAP with a helmet was successful in 69% of cases, with its use feasible for several days outside the ICU. It was evidenced in a study 29 that ELMOcpap failed in patients with moderate to severe hypoxemic respiratory failure caused by COVID-19 pneumonia. The authors reported that 55.4% of patients who avoided intubation and were then successfully weaned from CPAP to oxygen therapy. 29
A randomized clinical trial 30 which included patients with COVID-19 and moderate to severe AKI (PaO2/FIO2 < 200 mmHg) showed that NIV treatment with ELMOcpap, when compared to high-flow nasal oxygen (HFNO), it improved oxygenation, reduced dyspnea, reduced endotracheal intubation rate (OR = 0.41; 95%CI: 0.18-0.89; p = 0.03), and gradually increased the number of NIV-free days in 28 days: median = 28 days (IIQ: 13-28 days) vs. 25 days (IIQ: 4-28 days); p = 0.04. Despite these better results, NIV with ELMOcpap still did not reduce ICU mortality or hospital mortality when compared with HFNO. 31
Studies have shown that the effect of CPAP on the recruitment of swollen and/or collapsed alveoli is demonstrated with an immediate improvement in the ventilation/perfusion ratio (V/Q). 32,33 In addition, it can be seen that there was a reduction in respiratory rate, leading to a reduction in respiratory distress and an improvement in respiratory performance according to the ROX index ([SpO2/FIO2]/respiratory rate). Studies have shown that respiratory rate values below 24 bpm in a few hours with ELMOcpap were associated with greater efficacy in resolving hypoxemic respiratory failure. 34
In view of what was experienced in practice, patients who sought care late were unable to avoid orotracheal intubation (OTI), even with the application of the ELMOcpap helmet. It is evident that patients with hypoxemic respiratory failure resulting from complications of COVID-19 have a pathophysiological process similar to Acute Respiratory Distress Syndrome (ARDS), characterized by the most severe stage of the disease, in which many individuals require the use of invasive ventilatory support. 35
LIMITATION
Initially, the ELMO team composed of physicians, nurses and physiotherapists selected 28 patients, who completed an inclusion checklist. It should be noted that even before the pandemic, the ICU technical standard recommends 01 (one) physiotherapist for every 10 beds, which in a pre-pandemic scenario, it was reasonable since there were, on average, 2 patients with severely compromised lungs in a mixed ICU (postoperative, heart attacks, traumas, etc). In the pandemic, however, that number of patients rose to 10. That is, all ICU beds were practically occupied with seriously compromised lung patients. Given this fact, the sessions with physiotherapists were insufficient. 11
The relationship between the number of physiotherapists and the number of beds has a significant impact on the results of a survey like this one. Remembering that the work routines of the ICUs with regard to rehabilitation were not changed in relation to the general ICUs. That is, if there is no physical therapy consistent with the conditions of patients with acute lung impairment, the tendency for the clinical outcome is the worsening or death of the patient, which proves that rehabilitation is as important as ventilation.
CONCLUSÃO
The results of this study were based on 61 patients diagnosed with COVID-19, to assess its impact of ELMO helmet use on prominent outcomes such as length of hospital stay and intubation rates.
There were 28 patients who used ELMOcpap, there was an improvement in oxygenation parameters without, however, showing advantages over conventional treatment. The importance of rigorous respiratory monitoring and rehabilitation was highlighted.
What seems to have favored the patients was monitoring with respiratory physiotherapy, a procedure that was greatly impaired because there was no reform of the health teams in view of the new composition of the ICUs. That is, this issue of not having information about the composition of the ICU teams can compromise several studies.
REFERENCES
1 Borges, Daniel Lago, et al. "Posição prona no tratamento da insuficiência respiratória aguda na COVID-19." Assobrafir Ciência 11.Suplemento 1 (2020): 111-120.
2 Barauna, Luiz Henrique, and Fleury Ferreira Neto. "Uso da ventilação não invasiva na SDRA e pneumonia secundária a H1N1: revisão sistemática." Revista Pesquisa em Fisioterapia 9.3 (2019): 396-408.
3 Ferreira, Susana, et al. "Ventilação não invasiva." Revista Portuguesa de Pneumologia 15.4 (2009): 655-667.
4 Pinto, Ana Rita, et al. "Ventilação mecânica não invasiva e a severidade na disfunção temporomandibular em portadores de doença pulmonar obstrutiva crónica." Saúde & Tecnologia 21 (2019): 45-50.
5 Grinnan, Dc; Truwit, Jd. Clinical review: respiratory mechanics in spontaneous and assisted ventilation. Crit Care;9(5):472-84, 2005.
6 Klauer, Nr et al. Modeling Risk of ICU-Acquired Weakness in ARDS in a Randomized Clinical Trial of Helmet Ventilation. In: B104. Critical care: catch-22-beyond the ventilator: the challenges of delirium, icu-acquired weakness, and rehabilitation. American Thoracic Society, 2019.
7 Alencar, Airlane. Tipos de estudo e introdução à análise estatística. Instituto de, 2012.
8 Marconi, Marina de Andrade, and Eva Maria LAKATOS. "Metodologia de pesquisa." São Paulo: Atlas (2004).
9 Schettino, Guilherme PP, et al. "Ventilação mecânica não-invasiva com pressão positiva." Revista Brasileira de Terapia Intensiva 19.2 (2007): 245-257.
10 Gürbüz, ÖÇ et al. Comparison of helmet and facial mask during noninvasive ventilation in patients with acute exacerbation of chronic obstructive pulmonary disease: a randomized controlled study. Turk J Med Sci;45:600–6, 2015.
11 ANVISA. Agência Nacional. Novas Técnicas GVIMS/GGTES/ANVISA n° 04/2021. Orientações para serviços de saúde: medidas de prevenção e controle que devem ser adotadas durante a assistência aos casos suspeitos ou confirmados de infecção pelo novo coronavírus (SARS-CoV-2). Atualizada em 25/02/2021
12 Sinderby, Christer, et al. "An automated and standardized neural index to quantify patient-ventilator interaction." CriticalCare 17.5 (2013): 1-9.
13 LUCCHINI, Alberto et al. O “pacote de capacete” em pacientes com COVID-19 em ventilação não invasiva. Enfermagem em cuidados intensivos e críticos , 58:102859, 2020.
14 Holanda, Marcelo Alcantara. "UMA BRISA NO ELMO, UM SOPRO DE VIDA NA COVID-19." Cadernos ESP-Revista Científica da Escola de Saúde Pública do Ceará 15.2 (2021): 8-10.
15 Chang, Yao-Jen, Shu-Fang Chen, and Jun-Da Huang. "A Kinect-based system for physical rehabilitation: A pilot study for young adults with motor disabilities." Research in developmentaldisabilities 32.6 (2011): 2566-2570.
16 BRASIL, Ministério da Saúde, Conselho Nacional de Saúde. Resolução Nº 466, de 12 de Dezembro de 2012. Regulamenta diretrizes e normas regulamentadoras de pesquisas envolvendo seres humanos. Disponível em: http://www.ifpb.edu.br/reitoria/pro-reitorias/prpipg/comite-de-etica-em-pesquisa/documentos_cep/Resolucao%20no%20466-%20de%2012%20de%20dezembro%20de%202012.pdf/view. Acesso em Acesso em: 06 de abril de 2020.
17 Thomas, Sara, Celeste Alexander, and Bridget A. Cassady. "Nutrition risk prevalence and nutrition care recommendations for hospitalized and critically-ill patients with COVID-19." Clinical Nutrition ESPEN 44 (2021): 38-49.
18 Porto, Elias Ferreira, et al. "Mortalidade por Covid-19 no Brasil: perfil sociodemográfico das primeiras semanas." Research, Society and Development 10.1 (2021).
19 do Egypto Teixeira, Camila Melo, et al. "Análise comparativa das pandemias COVID-19 e H1N1." Brazilian Journal of Health Review 3.2 (2020): 3591-3595.
20 Zheng, Ying-Ying, et al. "COVID-19 and the cardiovascular system." Nature reviews cardiology 17.5 (2020): 259-260.
21 Centers for Disease Control and Prevention (CDC). (2020). Severe Outcomes Among Patients with Coronavirus Disease 2019 (COVID-19)-United States, 2020. Morbidity and Mortality Weekly Report (MMWR), 69(12), 343-346. https://www.cdc.gov/mmwr/volumes/69/wr/mm6912e2.htm. Acessoem: 18 de abril de 2022.
22 Martindale, Robert, et ai. "Terapia nutricional em pacientes criticamente doentes com doença de coronavírus 2019." Jornal de nutrição parenteral e enteral 44.7 (2020): 1174-1184.
23 Gupta, Shruti, et al. "Factors associated with death in critically ill patients with coronavirus disease 2019 in the US." JAMA internal medicine 180.11 (2020): 1436-1447.
24 Raith, Eamon P., et al. " Prognostic accuracy of the SOFA score, SIRS criteria, and qSOFA score for in-hospital mortality among adults with suspected infection admitted to the intensive care unit." Jama 317.3 (2017): 290-300.
25 Kovach, Christopher P., et al. "Comparative prognostic accuracy of sepsis scores for hospital mortality in adults with suspected infection in non-ICU and ICU at an academic public hospital." PloS one 14.9 (2019): e0222563.
26 Raschke, Robert A., et al. "Discriminant accuracy of the SOFA score for determining the probable mortality of patients with COVID-19 pneumonia requiring mechanical ventilation." Jama 325.14 (2021): 1469-1470.
27 Tomaz, Betina Santos, et al. "ELMO, uma nova interface do tipo capacete para CPAP no tratamento da insuficiência respiratória aguda hipoxêmica por COVID-19 fora da UTI: estudo de viabilidade." (2022): e20210349-e20210349.
28 Coppadoro, Andrea, et al. "Helmet CPAP to treat hypoxic pneumonia outside the ICU: an observational study during the COVID-19 outbreak." Critical Care 25.1 (2021): 1-10.
29 Aliberti, Stefano, et al. "Helmet CPAP treatment in patients with COVID-19 pneumonia: a multicentre cohort study." European Respiratory Journal 56.4 (2020).
30 Grieco, Domenico Luca, et al. "Effect of helmet noninvasive ventilation vs high-flow nasal oxygen on days free of respiratory support in patients with COVID-19 and moderate to severe hypoxemic respiratory failure: the HENIVOT randomized clinical trial." Jama 325.17 (2021): 1731-1743.
31 Valle, Bruno. "ELMO: uma interface inovadora para ventilação não invasiva." J Bras Pneumol 48.1 (2022): e20220005.
32 Li, Jinkui, et al. "Chest CT findings in patients with coronavirus disease 2019 (COVID-19): a comprehensive review." Diagnostic and Interventional Radiology 27.5 (2021): 621.
33 Cosentini, Roberto, et al. "Helmet continuous positive airway pressure vs oxygen therapy to improve oxygenation in community-acquired pneumonia: a randomized, controlled trial." Chest 138.1 (2010): 114-120.
34 Guo, Wei, et al. "A survey for COVID-19 among HIV/AIDS patients in two districts of Wuhan, China." AIDS Patients in Two Districts of Wuhan, China (3/4/2020) (2020).
35 Marques, Emanuela, Pereira Sales, and Janille Karem Moura. "FISIOTERAPIA, FUNCIONALIDADE E COVID-19: REVISÃO INTEGRATIVA."






