PSYCHOSOMATIC SYMPTOMS IN HEALTH PROFESSIONALS FIGHTING THE COVID PANDEMIC -19
RESUMO
A pandemia da covid-19 trouxe uma série de impactos a população mundial, principalmente, aos profissionais da saúde. OBJETIVO: Correlacionar o adoecimento psicossomático com estes impactos da covid-19 nos profissionais da linha de frente e evidenciar a necessidade de estratégias que promovam cuidados psicossociais. MÉTODO: Pesquisa de campo descritiva com estudo transversal qualitativo e quantitativo, com 31 profissionais da saúde, dos sexos masculino e feminino, maiores de 18 anos, de instituições de saúde pública e privada da cidade de São Luís-MA; dados coletados através de questionário on-line e análise de conteúdo segundo Bardin. RESULTADO: Percebeu-se que os profissionais de saúde que atuaram no enfrentamento da pandemia estão mais propensos a apresentar ou intensificar os sintomas psicossomáticos, impactando em sua saúde mental, com prejuízos na qualidade de vida. CONCLUSÃO:Há relação entre impactos gerados pela covid-19 e manifestações dos sintomas psicossomáticos, sendo necessário cuidados psicossociais a esses profissionais de saúde.
DESCRITORES: Saúde; Pandemia; Covid-19.
ABSTRACT
The covid-19 pandemic brought a series of impacts to the world's population, especially to health professionals. OBJECTIVE: To correlate psychosomatic illness with these impacts of covid-19 on frontline professionals and highlight the need for strategies that promote psychosocial care. METHOD: Descriptive field research with qualitative and quantitative cross-sectional study, with 31 health professionals, male and female, over 18 years old, from public and private health institutions in the city of São Luís-MA; data collected through an online questionnaire and content analysis according to Bardin. RESULT: It was noticed that health professionals who acted in the face of the pandemic are more likely to present or intensify psychosomatic symptoms, impacting their mental health, with damage to their quality of life. CONCLUSION: There is a relationship between impacts generated by covid-19 and manifestations of psychosomatic symptoms, requiring psychosocial care for these health professionals.
DESCRIPTORS: Health; Pandemic; Covid-19.
RESUMEN
La pandemia de covid-19 ha traído una serie de impactos a la población mundial, especialmente a los profesionales de la salud. OBJETIVO: Correlacionar la enfermedad psicosomática con estos impactos del covid-19 en los profesionales de primera línea y destacar la necesidad de estrategias que promuevan la atención psicosocial.MÉTODO: Investigación de campo descriptiva con estudio transversal cualitativo y cuantitativo, con 31 profesionales de salud, hombres y mujeres, mayores de 18 años, de instituciones de salud públicas y privadas de la ciudad de São Luís-MA; datos recolectados a través de cuestionario online y análisis de contenido según Bardin. RESULTADOS: Se observó que los profesionales de salud que trabajaron en el enfrentamiento de la pandemia son más propensos a presentar o intensificar síntomas psicosomáticos, impactando en su salud mental, con pérdidas en la calidad de vida. CONCLUSIÓN: Existe relación entre los impactos generados por el covid-19 y las manifestaciones de síntomas psicosomáticos, siendo necesaria la atención psicosocial de esos profesionales de salud.
DESCRIPTORES: Salud; Pandemia; Covid-19.
INTRODUCTION
This article was carried out through field research and aims to address the psychosomatic symptoms manifested to health professionals who acted on the front line in the fight against the covid-19 pandemic, specifically in the city of São Luís/MA, correlating with the impacts of the pandemic, as this subject has been the subject of discussion and has gained notoriety in worldwide research.
The coronavirus pandemic was officially declared by the World Health Organization (WHO) on January 23, 2020, due to the high percentage of case numbers in the short period in several countries, becoming one of the most serious illnesses of recent times, with damage to the physical and mental health of the population. (1-2)
At the level of Brazil (2020) it was in the city of São Paulo that the country had its first confirmed case of the coronavirus, thus evolving into a situation of seriousness and several unanswered questions. The Unified Health System (SUS) employed thousands of professionals, forming a first-line multidisciplinary team covering all areas, providing assistance to those infected. Until the registration of November 23, 2022, the country had 35,052,152 confirmed cases and 689,155 deaths, currently with 2% lethality. (3)
The main characteristic of the coronavirus is its high contagiousness, since transmission occurs through direct contact with respiratory particles, thus reproducing an acute respiratory syndrome, ranging from mild to very severe cases, with its lethality varying due to different clinical conditions, comorbidities and age range of individuals. (4) During the pandemic, it was recommended that preventive measures and actions with the drop in the number of cases continue, but the population reduced these precautions, due to the lack of adequate information. (5)
Health professionals who worked during the pandemic crisis were very vulnerable to the contamination of the virus due to direct assistance to positive patients, resulting in both psychological and physical consequences. (6) Coping actions impacted a large percentage of these professionals, who sustained long workdays until exhaustion and without prospects in the face of their arduous shifts, given the increase in the number of cases and deaths. There were episodes of professionals who presented symptoms of Covid-19 without being contaminated, thus observing psychosomatic symptoms.
Given this context, it is important to mention that mental health is not something restricted or even definitive, and refers to the psychological and emotional balance of the individual, being the ability to respond to everyday situations, through cognitive and emotional skills, providing balance and well-being to the individual. (7) In addition to society, health professionals showed signs and symptoms of anxiety and psychosomatic illnesses. (8) Several factors were prone to so many concerns and imbalances, such as: treating a disease that was not yet known, fear of infection and fear of spreading among their relatives, due to the care of those infected. (9) Added to this, the difficulty in dealing with grief, with the pain and suffering of others, are factors that triggered psychosomatic manifestations and the emergence of emotional suffering. The perception made by specialists alerts to the importance of taking care not only of the body, but of the emotions.
The discussion on which the article is based revolves around the biopsychosocial impacts of covid-19 being related to the emergence of psychosomatic symptoms and the illness process of health professionals.
METHOD
This is a descriptive field research with a quantitative and qualitative cross-sectional approach with 31 health professionals, aged between 18 and 51 years old, namely: nursing technicians, nurses, doctors, psychologists, social workers, physiotherapists, occupational therapists, pharmacists and the like, male and female, from various public and private health institutions in the city of São Luís-MA.
Data collection was performed using an online questionnaire developed using the GoogleForms® form (APPENDIX A), containing open and multiple-choice questions regarding sociodemographic data and the pandemic context and their association with the process of psychosomatic illness. In order to continue the answers, the professionals indicated that they worked on the front line of the fight against covid-19 specifically in the city of São Luís-MA.
The Form was available from November 3 to 12, 2022 on social networks: WhatsApp®, Facebook® and Instagram®; being sampled for convenience.
As inclusion criteria, the forms completely completed and answered by professionals who were on the frontline of the fight against Covid-19 and who worked in the city of São Luís-MA were considered for analysis; and exclusion were those residing in other cities and/or who answered incompletely.
The data analysis carried out was the content analysis according to Bardin's (2016) framework, directed at the impacts caused to health professionals who acted on the front line against the covid-19 pandemic. (10)
This study was submitted and approved by the Research Ethics Committee (CEP) CAAE: 63395722.0.0000.5084 of Universidade Ceuma de São Luís under opinion number: 5.681.343. Before data collection, participants signed the Free and Informed Consent Form (TCLE) (APPENDIX B) attached to the Google Forms® questionnaire, proving their acceptance to participate in the research, the disclosure, and publication of the results.
RESULTS
We obtained 31 responses, the results will be presented below:
According to the description data of the health professionals who worked to combat the Covid-19 pandemic, in the city of São Luís/MA, they are presented in Table 1. The health professionals who participated in this study, according to the sample, were predominantly female, 22 of them (71%) and the dominant age group among the participants was between 36 and 50 years 17 (55%), followed by professionals aged between 25 and 35 years 7 (23%) with a prevalence of single marital status. Still regarding the characterization of the professionals in this study, the majority 10 (32%) are psychologists; and health professionals with experience in their work from 01 to 05 years, 13 (42%) and soon after between 06 to 10, 10 (32%).
Table 1 - Characterization of health professionals who worked in the assistance of the covid-19 pandemic, in the city of São Luís/MA, 2022.
|
Gender |
No. |
% |
|
Female |
22 |
71 |
|
Male |
9 |
29 |
|
Other |
0 |
0 |
|
Age group |
No. |
% |
|
18 to 24 |
2 |
6 |
|
25 to 35 |
7 |
23 |
|
36 to 50 |
17 |
55 |
|
51 years of age and older |
5 |
16 |
|
Marital status |
No. |
% |
|
Single |
15 |
48 |
|
Married |
14 |
45 |
|
Divorced |
2 |
6 |
|
Widow (er) |
0 |
0 |
|
Other |
0 |
0 |
|
Function |
No. |
% |
|
Technician or Nursing Assistant |
5 |
16 |
|
Nurse |
5 |
16 |
|
Physician |
0 |
0 |
|
Psychologist |
10 |
32 |
|
Other |
11 |
35 |
|
Area of activity |
No. |
% |
|
Emergency or first aid |
4 |
13 |
|
Ambulatory (Elective Care) |
10 |
32 |
|
Inpatient Unit/Infirmary |
9 |
29 |
|
Intensive Care Unit (ICU) |
9 |
29 |
|
Transport of patients (ambulatory) |
2 |
6 |
|
Support service (imaging, diagnosis, etc.) |
2 |
6 |
|
Health system |
No. |
% |
|
Public |
17 |
55 |
|
Private |
9 |
29 |
|
Both |
5 |
16 |
|
Working time in the role |
No. |
% |
|
01 to 05 years |
13 |
42 |
|
06 to 10 years |
10 |
32 |
|
11 to 15 years |
2 |
6 |
|
16 years and more |
6 |
19 |
|
Time working on the front line of the covid-19 pandemic |
Nº |
% |
|
01 to 06 months |
7 |
23 |
|
07 to 12 months |
8 |
26 |
|
More than 01 year |
15 |
48 |
|
Sporadic time |
1 |
3 |
Source: Prepared by the author based on research data, 2022
The form included some professional classes in the health area, which were 5 (16%) Nursing Technicians or Assistants, 5 (16%) Nurses, 10 (32%) Psychologists and others with 11 (35%) between the functions of Nurse and Rescuer of the Fire Department, Occupational Therapist, Occupational Safety Engineer, Physiotherapist, Human Resources Manager and Social Worker. It is important to note that 13 (42%) of the professionals were infected with covid-19 during the first wave.
Also in table 1, it can be seen that the areas of activity of health professionals were prevalent in outpatient clinics (Elective Care), Inpatient Unit/Infirmary and Intensive Care Unit (ICU/ICU) and most 17 (55%) of these professionals worked in the public health system. Another data in table 1 was the period of action to combat the coronavirus with the dominant percentage of 15 (48%) who remained over 01 (one) year of pandemic confrontation.
Some difficulties faced by research participants in the workplace during the first wave of the Covid-19 pandemic:
Lack of infrastructure. Lack of medicines. Having contacts with people with covid and seeing people who died. Lack of PPE. Wearing a mask for a long period of time. The fact that the professionals themselves are affected by the disease. Fear. Insecurity. Lack of support from superiors. Work overload, low level of management training.
In Graph 1, in terms of physical symptoms, the most common changes were muscle pain (14 responses), insomnia (11 responses), constant headaches (10 responses), fast heartbeats (06 responses), feeling of suffocation or shortness of breath and/or chest pain (05 responses) and complaints of generalized pain (05 responses).
Graph 1 – Physical symptoms presented in the work on the frontline of covid-19, 2022.
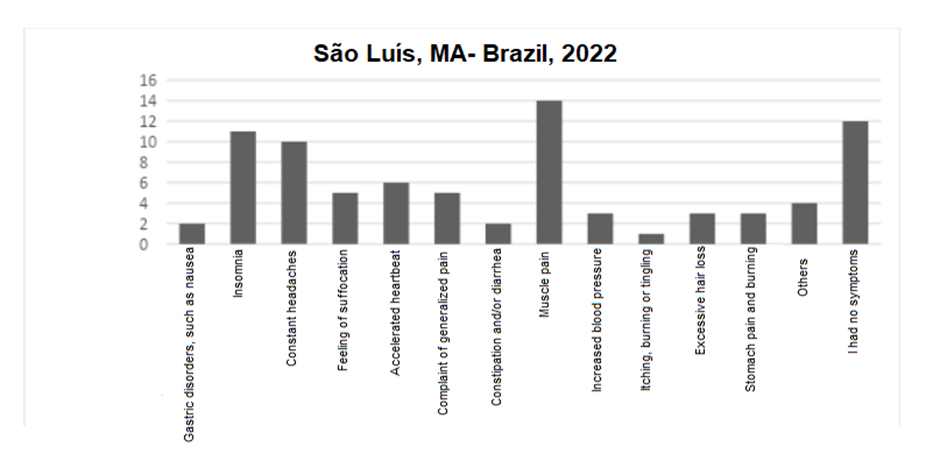
Source: Prepared by the author based on research data, 2022.
Graph 2 shows the health conditions related to the emotional symptoms presented during work on the front lines of the new coronavirus. Among the participants, the alleged emotional symptoms were anxiety (17 responses), sadness (17 responses), impatience (09 responses) and irritability (07 responses).
Graph 2 – Emotional symptoms presented in front-line performance of Covid-19, 2022.
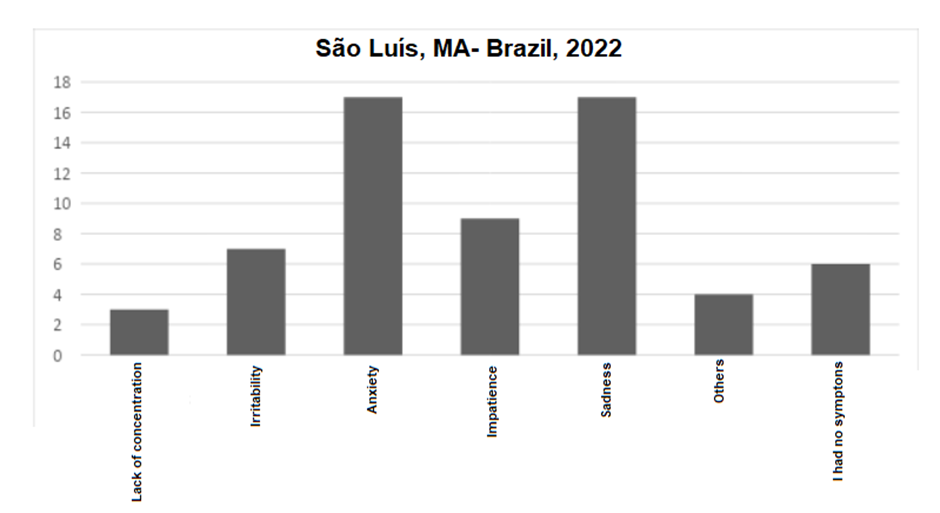
Source: Prepared by the author based on research data, 2022.
There is a discrepancy between the period in which they presented physical and/or emotional symptoms, 10 (32%) of the participants reported that they felt the symptoms for less than 01 month and 09 (29%) already reported that they had the symptoms for more than 01 (one) year.
The highest percentage of participants did not obtain psychological or psychiatric follow-up, with (11 responses) saying no, for other reasons and (08 responses) reporting no, as these services were not available.
When evaluating the answers, we saw that, when asked about the impacts in the professional scope, the most significant reports:
I work on a small scale, discovering the importance of my profession in an ICU, having to deal with people suffocating and dying so quickly, not being able to alleviate that situation, the impotence of not being able to do anything in front of positive people, the late adherence to the use of a mask and social distance, it was knowing that some people came in, talking , walking and then dying, The large number of deaths was a striking factor.
And regarding the impact on a personal level, but relevant:
O medo de contaminar meus familiares. O medo da possibilidade de estar levando a doença para minha família, a exaustão por conta do trabalho excessivo, a sensação de impotência diante de tantas perdas e o distanciamento das pessoas amadas. A incerteza sobre o amanhã, a angústia pela espera da vacina. Assim como o sofrimento do outro, e ao mesmo tempo a possibilidade de ajudar o próximo diante do desconhecido. Era gratificante saber que ajudamos vidas, dando apoio e esperança. Perda de pessoas próximas. O medo constante de pegar a doença e contaminar algum familiar meu.
According to this research, physical and emotional symptoms harmful to the mental health of those who worked in the care of patients infected with the coronavirus were detected.
DISCUSSION
According to the data presented in the results of this research regarding the health conditions correlated to the physical symptoms in the performance of the health professional on the frontline of the coronavirus, those significantly scored were muscle pain; insomnia; constant headaches; rapid heartbeat; feeling suffocated or short of breath and/or chest pain; and complaints of generalized pain and as emotional symptoms presented with a higher percentage that were anxiety; sadness; impatience; and irritability. (11)
From this, the process of triggering the manifestations of psychosomatic symptoms becomes evident, because these symptoms are correlated with feelings, the way of thinking and also the control of emotions. Negative thoughts and uncontrolled emotions can trigger mental imbalances, overloading organic functions and impairing the functioning of the body. (12)
As for the characterization of the professionals, the data reveal the dominance of the female gender, leading us to deduce that in fact, in recent decades, women have been working in the health area. The performance of women health professionals on the front line of the fight against the coronavirus represented 70% worldwide. (13)
Regarding the research, there was also an impact on the personal scope of health professionals, since there was the possibility of contamination of their family members, a feeling of impotence and, above all, the uncertainty of the following days. The large number of deaths was an important factor to accentuate the psychosomatic symptoms presented by the team.
According to Fiocruz research (2021) the results proved that health professionals who worked in the care of patients contaminated by covid-19 had harmful consequences for mental health. These professionals dealt with very difficult situations for a long time, such as increased workload, new protocols, loss of patients, complexity of disease severity levels, lack of material resources such as personal protective equipment and many other challenges faced by health professionals who worked on the front lines of the fight against the coronavirus that can intensify or trigger the manifestations of psychosomatic symptoms, anxiety, depression. (14)
Undoubtedly, this milestone in history that is covid-19 will need to be studied for many years, to analyze the short- and long-term mental health consequences.
CONCLUSION
It is inferred from the data of the present research that there is an interaction of the impacts generated by the covid-19 pandemic with the manifestations of psychosomatic symptoms in health professionals who worked on the front line of the fight against the Covid-19 pandemic in São Luís / MA .
The limitations found in this study were the unavailability of several professionals due to the increase in new cases of covid-19 in the city, making it difficult for the research to reach this sample.
The importance of further research on the covid-19 pandemic is highlighted, with the intention of analyzing the short- and long-term mental health consequences of these professionals who were reluctant to face a devastating virus.
Finally, this research intends to bring reflection and discussion in public policies on strategies that promote more psychosocial care actions to these professionals in a timely and assertive manner, to face the impacts of the coronavirus pandemic on health professionals who worked on the front lines of the fight against covid-19.
REFERENCES
- SAIDEL MGB, Lima MH de M, Campos CJG, Loyola CMD, Espiridião E, Rodrigues J. Intervenções em saúde mental para profissionais de saúde frente a pandemia de Coronavírus. Revista Enfermagem UERJ. 21 de maio de 2020;28(0):49923.
- HELIOTERIO MC, Lopes FQR de S, Sousa CC de, Souza F de O, Pinho P de S, Sousa FN e F de, et al. Covid-19: Por que a proteção de trabalhadores e trabalhadoras da saúde é prioritária no combate à pandemia? Trabeduc saúde. 2020;18(3):e00289121.
- Saúde mental: pesquisa analisa impacto psicológico do enfrentamento à Covid-19 em profissionais da saúde [Internet]. Casa Civil.
- GRINCENKOV FR. A Psicologia Hospitalar e da Saúde no enfrentamento do coronavírus: necessidade e proposta de atuação. HU Revista. 8 de abril de 2020;46:1–2.
- Segunda onda de covid-19 no Brasil [Internet]. Brasil Escola. [citado 6 de janeiro de 2023]. Disponível em: https://brasilescola.uol.com.br/doencas/segunda-onda-de-covid-19-no-brasil.htm
- TEIXEIRA CF de S, Soares CM, Souza EA, Lisboa ES, Pinto IC de M, Andrade LR de, et al. A saúde dos profissionais de saúde no enfrentamento da pandemia de Covid-19. Ciênc saúde coletiva. 28 de agosto de 2020;25:3465–74.
- LUCCA SR de. SAÚDE, SAÚDE MENTAL, TRABALHO E SUBJETIVIDADE. Revista Laborativa. 1o de abril de 2017;6(1 esp):147–59.
- SOUZA, M. N., & Almeida, M. P. P. M. Incidência de sintomas de ansiedade em profissionais da área da saúde atuantes no combate à pandemia da Covid-19. Psicologia-Tubarão.
- COVID-19 em profissionais da saúde, vivências e perspectivas: um relato de experiência | Revista Eletrônica Acervo Saúde. 22 de dezembro de 2020 [citado 6 de janeiro de 2023];
- BARDIN, L. Análise de Conteúdo. São Paulo: Edições 70, 3ª reimpressão da 1ª edição, 2016.
- FIOCRUZ. 2021. Disponível em: https://portal.fiocruz.br/noticia/pesquisa-analisa-o-impacto-da-pandemia-entre-profissionais-de-saude. Acesso em: 11 de nov. 2022.
- MÔNICA HS. Entenda o que são doenças psicossomáticas: qual a origem, sintomas e tratamentos [Internet]. Hospital Santa Mônica. 2019 [citado 12 de janeiro de 2023]. Disponível em: https://hospitalsantamonica.com.br/entenda-o-que-sao-doencas-psicossomaticas-qual-a-origem-sintomas-e-tratamentos/.
- POLAKIEWICZ R. Mulheres na linha de frente do combate à Covid-19 [Internet]. PEBMED. 2020 [citado 12 de janeiro de 2023]. Disponível em: https://pebmed.com.br/mulheres-na-linha-de-frente-do-combate-a-covid-19/
- BEZERRA GD, Sena ASR, Braga ST, Santos MEN dos, Correia LFR, Clementino KM de F, et al. O impacto da pandemia por COVID-19 na saúde mental dos profissionais de saúde: revisão integrativa. Revista Enfermagem Atual In Derme. 4 de setembro de 2020;93:e-020012.