Proposal for monitoringpatientswith diabetes mellitus type 2: a cluster analysis.
RESUMO
Objetivo: Analisar fatores associados ao controle glicêmico de pacientes com diabetes mellitus tipo 2 (DM2). Métodos: estudo transversal de base populacional, fonte de dados e registros de prontuários. Os participantes foram descritos segundo as informações sociodemográficas, clínicas e comportamentais em relação ao controle glicêmico. Realizado análise de cluster do tipo hierárquico, utilizando o método de similaridade de Jaccard. Resultados: analisados prontuários de 605, dos quais 270 (44,6%) não tinham bom controle glicêmico, 396 (65,4%) tinham acima de 60 anos e 361 (59,7%) eram mulheres. A análise de cluster discriminou quatro grupos de indivíduos agrupados por sua similaridade, em relação ao colesterol total e triglicérides, variáveis que melhor discriminaram os grupos. Conclusão: A maioria eram mulheres, idosos, acima do peso e um alto percentual de pessoas com mau controle glicêmico.
Descritores: Diabetes Mellitus; Atenção Primária à Saúde; Controle Glicêmico; Estudo observacional.
ABSTRACT
Objective: To analyze factors associated with glycemic control in patients with diabetes mellitus type 2 (DM2). Methods: It is a cross-sectional study population-based using medical records as a data source. Participants were described according to their sociodemographic, clinical and behavioral characteristics and regarding their glycemic control. Subsequently, a hierarchical cluster analysis was carried out, using the Jaccard similarity method. Results: 605 medical records were analyzed, among them 270 (44.6%) did not have a good glycemic control, 396 (65.4%) were over 60 years old and 361 (59.7%) were women. Cluster analysis discriminated four groups of individuals grouped by their similarity, mainly in relation to the total cholesterol and triglycerides, variables that best discriminated the groups. Conclusion: Most participants were women, elderly, overweight and a high percentage of people without glycemic control.
DESCRIPTORS: Diabetes Mellitus, HeathPrimarycare, Glycemic control, Observational study
RESUMEN
Objetivo: analizarlos factores asociados con el control glucémico de pacientes con diabetes mellitus tipo 2 (DM2). Métodos: estudio cruzado basado en la población, fuente de datos Los registros de registros médicos. Los participantes fueron descritos de acuerdo con la conformación sociodemográfica, clínica y conductual sobre el control glucémico. Realizado análisis de clúster jerárquico, utilizando el método de similitud de Jaccard. Resultados: los registros médicos analizados de 605, de los cuales 270 (44.6%) no tenían un buen control glucémico, 396 (65.4%) tenían más de 60 años y 361 (59.7%) eran mujeres. El análisis de grupos discriminados contra cuatro grupos de individuos agrupados por su similitud, en relación con el colesterol total y los triglicéridos, variables que mejor discriminan a los grupos. Conclusión: La mayoría eran mujeres, ancianos, sobrepeso y un alto porcentaje de personas con mal control glucémico.
Descriptores: Diabetes mellitus; Primeros Auxilios; Control Glicémico; Estudio observacional.
INTRODUCTION
Like other non-communicable chronic diseases, diabetes mellitus (DM), especially type 2 (DM2), has shown an epidemiological rise in recent years. This has been a major challenge for public health, since the multifactorial etiology of this disease requires services to have an expanded approach to patients. 1
Data from the International Diabetes Federation 2 estimate that around 537 million adults between 20 and 79 years old live with DM, which represents 10.5% of the world population in this age group. The perspectives for the future show that in 2030 diabetes may affect 642.7 million people (11.3%) and 783.2 million adults in 2045 (12.2%). Among children and adolescents (under 20 years old) the disease affects approximately 1.2 million. Hyperglycemia already affects one in six pregnant women and the direct expenditure on diabetes in the world already approaches one trillion dollars. Brazil is the sixth country with the highest number of adults with DM (15.7 million) behind only China, India, Pakistan, United States and Indonesia, but the third with the highest expenses due to the DM, 42.9 billion dollars in 2021. 2
According to the latest survey by Surveillance of Risk and Protective Factors for Chronic Diseases by Telephone Survey (Vigitel) 3, carried out in 27 Brazilian capitals with adults (over 18 years old), there is a declared national prevalence of 9.1% of people with DM, in Belo Horizonte this number was 11.3%. The frequency is higher among women (9.6%) than among men (8.6%) with a tendency to increase with advancing age. It is interesting to note that the higher the level of education, the lower the frequency of DM. 3 Study carried out by Nilson et al. 4 pointed out that hospitalizations attributed to arterial hypertension, diabetes and obesity, in 2018, generated a cost to the Unified Health System (SUS) of 3.84 billion reais; 30% of this value refers to diabetes.
Considering the importance of DM as a public health problem, several institutions and societies have created guides and/or guidelines 1,2,5,6. These can be considered as a compilation of information based on robust scientific evidence and aimed at directing care. 5 However, the practical application of this information has proven to be a challenge for public health, as it depends on good patient adherence and specific knowledge on the part of professionals. 5 The adoption of other tools such as the Food Guide for the Brazilian Population 7 and the Collective Approach Instruction for the Management of Obesity in Primary Health Care 8 complement the guidance capacity of professionals and can help in the treatment and self-care by the patient. Several studies in Brazil have shown that, in their populations, a significant portion of patients with diabetes cannot maintain good glycemic control, which increases the risk of complications and increased mortality. 9–11
The objective of this study was to describe patients with DM2 treated in primary health care in the municipality, to evaluate the associations between sociodemographic parameters, biochemical factors and use of the health service with their glycemic control and group them according to the risk profile. It is expected that, by knowing the profile of this population and the factors associated with glycemic control, health professionals and managers will be able to expand their decision-making capacity and improve service to users.
METHODS
This is a cross-sectional, population-based study using a secondary data source, carried out in a municipality with approximately 22,000 inhabitants in the central-west region of Minas Gerais. The Strengthening the Reporting of Observational Studies in Epidemiology – STROBE tool was adopted in all stages of the work.
The study population consisted of all patients with DM2, aged 18 years or older, registered in the eight municipal Family Health Strategy (FHS) units. The exclusion criteria adopted were individuals with cognitive impairment and/or living at home, considering that they did not have full independence over their treatment. The cognitive and physical condition has already been informed a priori by the health team responsible for the patient.
It consisted of obtaining secondary data (gender, age, marital status and race; clinical data, body mass index (BMI), biochemical tests and type of drug treatment adopted; of use of the health service such as participation in groups, assessment of the fundus of the eye and feet and referral to other services). In order to guarantee a better quality of the information collected and to avoid information bias, the data were recorded in a Structured Collection Instrument, created by the authors, to obtain sociodemographic, clinical and behavioral information of patients with DM2 duly registered in each health unit. Such information was extracted from the following documents: family risk stratification, citizen's individual medical record, medication record and hypertensive and/or diabetic registration form in Hiperdia. These data were collected using the Questionnaire Design Study (QDS) and Excel® program, from August 2019 to November 2020. Data analysis was performed using the Excel® and Stata 17.0 programs in the year 2021.
A pilot study was previously carried out in an FHS unit to test the adequacy of all instruments and procedures contained in the methodology, with a view to enabling adaptations that were necessary before definitive data collection.
The history of attendance or absence at appointments was obtained from the record of missed appointments in medical records, with date and professional specialty. Previously canceled consultations were excluded. To verify the presence of patients in operative groups or collective activities with a related theme, we used the record of actions in the computerized system used by the municipality. Those who participated in at least one class action were identified as participants and those who had no record in the period were identified as non-participants.
For the physical activity group variable, we had the support of the Physical Educator of the Expanded Family Health Center (Nasf) who directed us to the records, both manual and computerized, used in the municipality. Those who participated at some point in the physical exercise groups were identified as participants and those who had no record were identified as non-participants.
For BMI, the classification was considered: underweight, eutrophic and overweight (overweight for the elderly and overweight plus obesity in adult patients) according to the classification adopted by the Ministry of Health. 12
Glycated hemoglobin (HbA1c) was the variable considered dependent (outcome). The American Diabetes Association (ADA) classification was used 1 and according to its value, the patient was classified as controlled or not. It was considered as good diabetes control (HbA1c <7.5%) and poor control (HbA1c≥ 7.5%) from the last measurement during the study period. When the patient did not present this data, fasting blood glucose (FG) was used, considered as adequate diabetes control (FG between 80-130mg/dl) and inadequate control (FG>130mg/dl).
Continuous variables were described according to mean, median and standard deviation or categorized to facilitate presentation in tables. Ordinal variables were described according to proportion.
A hierarchical cluster analysis was developed, using the Jaccard similarity method, which included the following categorical variables: Body Mass Index (BMI), total cholesterol, triglycerides and glycemic adequacy classification, as proposed by the ADA.
RESULTS
According to the Municipal Health Department, in 2019, 834 patients aged 18 years and over with DM2 were registered in primary health care. Patients with cognitive impairment (n=74) or those living at home (n=81) were excluded. The cognitive and physical condition was informed a priori by the health team responsible for the patient. Additionally, 74 records (8.87%) were not available during the collection period due to several factors, such as: possible change of address, death and patients who, although registered, do not use the service. Therefore, the present study evaluated the medical records of 605 users, and 251 (41.49%) patients had controlled blood glucose, 270 (44.63%) did not have good control and information on blood glucose was not available in 84 records (13.88%). Regarding sociodemographic data, 361 participants were women (59.60%), 255 (51.27%) declared themselves white, 396 elderly over 60 years old (65.45%) and 379 married or living with a partner (62.64%) (Table 1). No significant differences were observed between the variables, except in relation to gender.
Table 1 – Sociodemographic variables of patients with DM2 enrolled in Primary Health Care in a small town in the interior of Minas Gerais, 2022.
|
Variable |
Proper Control |
Without control |
Without classification |
Total |
P value * |
|
|
N=251(41,5%) |
N=270(44,6%) |
N=84(13,9%) |
N=605(100%) |
|||
|
|
SOCIODEMOGRAPHIC VARIABLES |
|||||
|
Sex |
|
|
|
|
|
|
|
Female |
173 (68,92) |
143 (52,96) |
45 (53,57) |
361 (59,67) |
|
|
|
Male |
78 (31,08) |
127 (47,04) |
39 (46,43) |
244 (40,33) |
0,001 |
|
|
Age |
|
|
|
|
|
|
|
22 – 60 years |
72 (28,69) |
102 (37,78) |
35 (41,67) |
209 (34,55) |
|
|
|
61 – 70 years |
90 (35,86) |
82 (30,37) |
25 (29,76) |
197 (32,56) |
|
|
|
71 – 93 years |
89 (35,46) |
86 (31,85) |
24 (28,57) |
199 (32,89) |
0,086 |
|
|
Marital Status |
|
|
|
|
|
|
|
Married/Living together with someone |
161 (64,14) |
163 (60,37) |
55 (65,48) |
379 (62,64) |
|
|
|
Others |
25 (9,96) |
38 (14,07) |
10 (11,9) |
73 (12,07) |
0,146 |
|
|
Without info |
65 (25,90) |
69 (25,56) |
19 (22,62) |
153 (25,29) |
|
|
|
Skin color |
|
|
|
|
|
|
|
White |
54 (21,51) |
67 (24,81) |
10 (11,90) |
131 (21,65) |
|
|
|
Black |
25 (9,96) |
19(7,04) |
5 (5,95) |
49 (8,10) |
|
|
|
Brown |
33 (13,15) |
29 (10,74) |
11 (13,10) |
73 (12,07) |
|
|
|
Other |
0 |
2 (0,74) |
0 |
2 (0,33) |
0,225 |
|
|
Without info |
139 (55,38) |
153 (56,67) |
58 (69,05) |
350 (57,85) |
|
|
* Chi-square test – excluding the “missing”
Source: Survey data, 2022
Table 2 presents the clinical variables in relation to glycemic control. In 592 (97.85%) it was possible to classify the nutritional status through BMI, and 423 (69.92%) patients were overweight. Of those who had a record of biochemical tests, 265 had good glycemic control (HbA1c <7.5) (58.24%), 304 had total cholesterol below 200 mg/dL (62.94%), HDL below 60 (n=356; 75.74%), LDL below 100 mg/dL (n=115; 52.04%), triglycerides below 150 mg/dL (n=256; 53.44). With regard to drug treatment, most patients use medications not associated with insulin therapy (n=438; 72.40%), 599 had no record of fundus examination (99.01%), 594 had no foot assessment (98.18%) and 563 (93.06%) had no record of referral to the Hiperdia Program reference center , currently the State Center for Specialized Care (CEAE).
Table 2 – Clinical variables of patients with DM2 enrolled in Primary Health Care in a small town in the interior of Minas Gerais, 2022.
|
Variable |
Proper Control |
Without control |
Without classification |
P value * |
|
N=251(41,5%) |
N=270(44,6%) |
N=84(13,9%)
|
||
|
CLINICAL VARIABLES |
||||
|
BMI |
|
|
|
|
|
Low weight |
16 (6,37) |
11 (4,07) |
5 (5,95) |
|
|
Eutrophic |
56(22,31) |
69(25,56) |
12(14,29) |
|
|
Overweight /obesity |
178(70,92) |
187(69,26) |
58(60,05) |
0,379 |
|
No information |
1 (0,40) |
3 (1,11) |
9 (10,71) |
|
|
Glycated hemoglobin |
|
|
|
|
|
<5.7 |
18 (7,17) |
2 (0,74) |
1 (1,19) |
|
|
5.7 to 6.5 |
91 (36,25) |
25 (9,26) |
1(1,19) |
|
|
6.5 to 7.5 |
73(29,08) |
53 (19,63) |
1(1,19) |
|
|
7.5 to 9.0 |
29 (11,55) |
67(24,81) |
1 (1,19) |
|
|
9 or higher |
8 (3,19) |
82 (30,37) |
3 (3,57) |
0,001 |
|
Without results |
32 (12,75) |
41 (15,19) |
77(91,67) |
|
|
Total cholesterol |
|
|
|
|
|
<200 |
165 (65,74) |
136 (50,37) |
3 (3,57) |
|
|
200-239 |
56 (22,31) |
61 (22,59) |
5(5,95) |
|
|
240 or higher |
14 (5,58) |
42 (15,56) |
1 (1,19) |
0,001 |
|
Without results |
16 (6,37) |
31 (11,48) |
75 (89,29) |
|
|
HDL |
|
|
|
|
|
<40 |
40 (15,94) |
54 (20.00) |
1 (1,19) |
|
|
40 a 60 |
130 (51,79) |
126 (46.67) |
5 (5,95) |
|
|
60 ou maior |
59 (23,51) |
53(19.63) |
2 (2,38) |
0,296 |
|
Without results |
22 (8,76) |
37(13.70) |
76 (90,48) |
|
|
LDL |
|
|
|
|
|
<100 |
65 (25,90) |
48(17,78) |
2 (2,38) |
|
|
100-129 |
23 (9,16) |
33(12,22) |
2(2,38) |
|
|
130-159 |
12 (4,78) |
16(5,93) |
0 |
|
|
160-189 |
7(2,79) |
9(3,33) |
0 |
|
|
190 ou maior |
0 |
4(1,48) |
0 |
0,058 |
|
Without results |
144(57,37) |
160 (59,26) |
80 (95,24) |
|
|
Triglicérides |
|
|
|
|
|
<150 |
138 (54,98) |
114 (42,22) |
4 (4,76) |
|
|
150<200 |
46 (18,33) |
34 (12,59) |
1 (1,19) |
|
|
200 <500 |
46 (18,33) |
82 (30,37) |
3 (3,57) |
|
|
500 ou maior |
2 (0,80) |
9 (3,33) |
0 |
0,001 |
|
Without results |
19 (7,57) |
31 (11,48) |
76 (90,48) |
|
|
Specific treatment |
|
|
|
|
|
No treatment |
2 (0,80) |
5 (1,85) |
1 (1,19) |
|
|
Just hypoglycemic |
196 (78,09) |
171 (63,33) |
61(72,62) |
|
|
Insulin only |
3(1,20) |
12 (4,44) |
3(3,57) |
|
|
Both |
40 (15,94) |
77(28,52) |
14(16,67) |
0,001 |
|
Without information |
10 (3,98) |
5 (1,85) |
5 (5,95) |
|
|
Fundus eye exam |
|
|
|
|
|
No |
247 (98,41) |
268(99,26) |
84(100,00) |
|
|
Yes |
4(1,59) |
2(0,74) |
0 |
0,362 |
|
Feet Assessment |
|
|
|
|
|
No |
245 (97,61) |
266(98,52) |
83(98,81) |
|
|
Yes |
6(2,39) |
4(1,48) |
1 (1,19) |
0,450 |
|
Hiperdia Forwarding |
|
|
|
|
|
No |
225 (89,64) |
232(85,93) |
76 (90,48) |
|
|
Yes |
26(10,36) |
38(14,07) |
8(9,52) |
0,197 |
* Chi-square test – excluding the “missing”
Source: Survey data, 2022
Figure 1 demonstrates the numerical distribution of individuals in four groups created from the cluster analysis. These groups are exclusive, that is, each individual is present in only one group.
Figure 1. Dendrogram of numerical distribution of patients with DM2 grouped from cluster analysis, 2022.
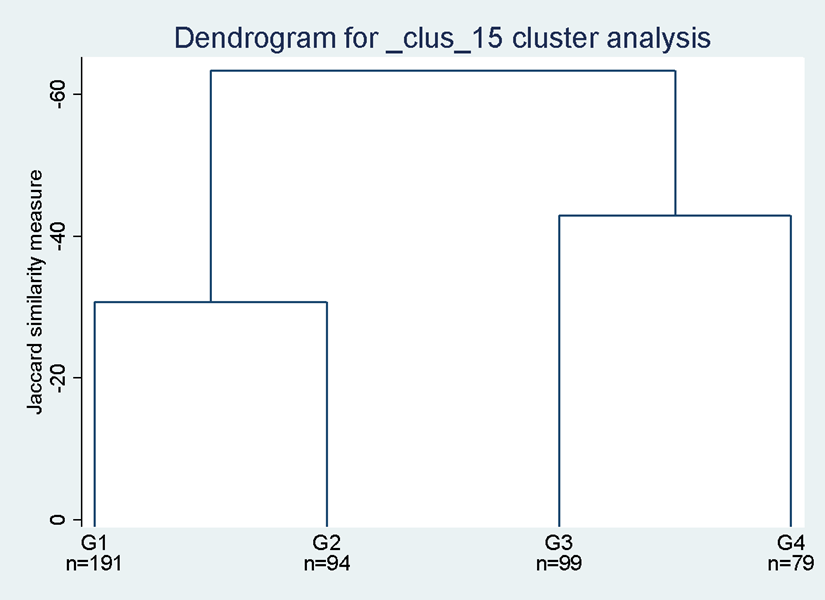
Fonte: Dados da pesquisa, 2022.
Figure 2 shows a box plot with the variables BMI, triglycerides and total cholesterol according to glycemic control and the group to which patients were allocated by cluster analysis.
Figure 2 - Box plot graph with BMI, triglycerides and total cholesterol variables according to glycemic control and the group to which the patient was allocated by cluster analysis, 2022.
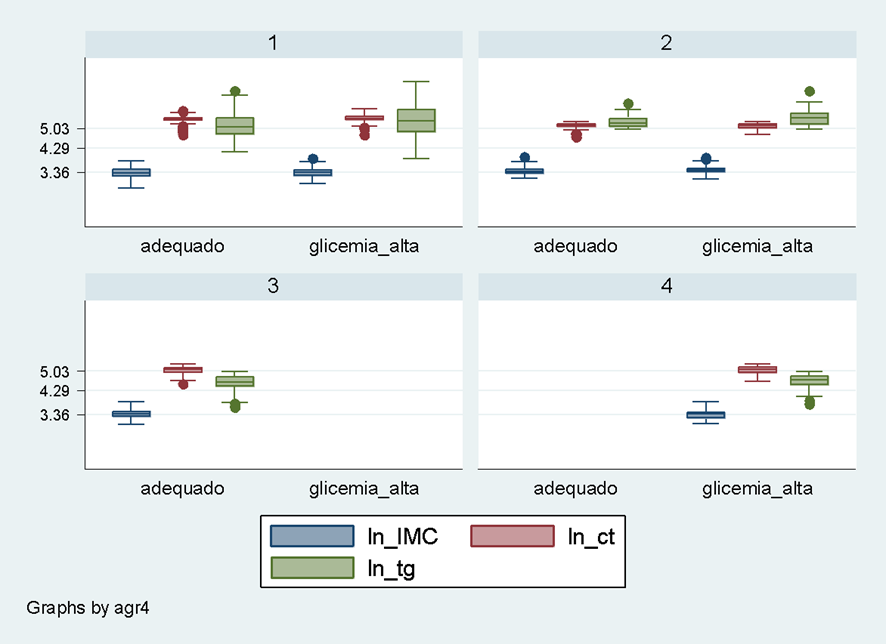
Source: Research data, 2022.
Group 1 presents greater heterogeneity among its individuals, including individuals with good and poor glycemic control. The BMI presents similarity in the individuals in both cases, while the values of triglycerides and total cholesterol tend to present values considered high. Group 2 is also formed by individuals with good and poor blood glucose control. In this group, the BMI variation showed no difference, but triglycerides and total cholesterol values are higher. Group 3 was composed only of individuals with good glycemic control, eutrophic or overweight BMI, high total cholesterol and low triglycerides. Group 4 is formed by individuals with poor glycemic control, BMI ranging from eutrophic to overweight, high total cholesterol, but low triglycerides. This distribution is better detailed in Table 1.
Chart 1 - Characteristics of patients with DM2 distributed in the 4 groups organized by cluster analysis, 2022.
|
Group |
BMI (median, P75, IQR*) |
Total Cholesterol |
Triglycerides |
ADA |
N |
|
1 |
0,1 or 2 (28,7;33,2; 8,7) |
Medium (219;235;29) |
Medium (162;236;114) |
0 |
82 |
|
2 |
1 or 2 (29,7;32,9;5,7) |
Low (170,187;27) |
Medium (186,233;70) |
0 |
47 |
|
3 |
1 or 2 (29,7;33,6;7) |
Low (162;176;34) |
Low |
0 |
99 |
|
4 |
|
|
|
|
0 |
|
1 |
0,1 or 2 (28,6;32,5;7,7) |
Medium (225;251;40) |
High |
1 |
109 |
|
2 |
1 or 2 (31,64;34,6;6,2) |
Low (174;187;35) |
High(230;284;108) |
1 |
47 |
|
3 |
|
|
|
|
0 |
|
4 |
1 or 2 (29,26;31,9;7,4) |
Low (162;182;61) |
Low |
1 |
79 |
*Interquartil Range
Source: Research data, 2022.
DISCUSSION
Among the variables collected, gender, HbA1C, total cholesterol, triglycerides and type of treatment were statistically associated with glycemic control. The variables total cholesterol and triglycerides showed better ability to discriminate between groups. Almost half of the patients (44.6%) did not have adequate glycemic control. Among participants who had adequate glycemic control (≈44%), most were female and over 60 years old (71.3%). Similar results were found by Muzi et al., 9 when crossing data from three official surveys of national representation in which they estimated a prevalence of 9.2% of DM in Brazil and, among women, this prevalence (10.2%) was higher than that of males (8.1%) and also that, in general, most participants (57.2%) had poor glycemic control. By evaluating the biochemical profile of 776 patients with diabetes from a laboratory in southern Brazil, Fiuza et al.10 found that 61.5% were female, 58% were over 60 years of age, and that the general mean values of triglycerides, glycemia, and HbA1c of all participants were above the recommended level.
Regarding BMI, approximately 70% of patients were overweight, a percentage higher than that found in the Brazilian adult population, which, in 2021, was 55.7%13. Lyra's work 11 which evaluated 2000 diabetic patients in Teresina/PI found 78.6% of overweight people and 56.2% of sedentary people in their study population. Although this research did not find a statistical association between BMI and glycemic control, the literature points to overweight as a factor strongly linked to DM2. 1,2,8 A possible cause to explain this lack of association is the low BMI variability in the variable studied, given that the vast majority of participants were above the recommended weight, which partly contributes to the non-differentiation between patients with good and poor glycemic control. The high prevalence of overweight in our study population may be associated with inadequate lifestyle habits, common throughout most of Brazil, such as reduced physical activity, both at work and during leisure, and excessive consumption of ultra-processed foods. It is known that, in recent decades, the consumption of these foods has more than doubled; a fact that can be explained by its practicality, palatability, durability and, often with commercial advantage over in natural foods and heavy marketing of industries.14 The reduction in the consumption of fruits and vegetables can also be influenced by factors such as accessibility, price, knowledge, convenience, organoleptic characteristics, among others. 15
The prescription and proper use of medication are also key factors in the treatment of DM2(5). In this study, we noticed that the number of patients who use insulin (32.96%) or who do not use any medication (1.85%) is higher among users without control, when compared to people who have good control and who use insulin (17.14%) or do not use medication (0.80%) and have good glycemic control. This finding may be the result of two important factors, the first referring to adherence to treatment and the second to access to necessary medications. Adherence is known to be affected by a number of factors, such as economic and social issues 16 and that the SUS supplies the medicines, but it is not uncommon for shortages to be recorded. 9 Understanding the reasons that may explain the lack of DM2 control in these patients is essential.
Another fact that draws attention is the low percentage of patients who underwent annual evaluation of the feet and examination of the fundus of the eye, because, although it is a recommendation of the Brazilian Society of Diabetes (SBD - Sociedade Brasileira de Diabetes) 5, only a minimal percentage of patients had these records in their medical records. Our results corroborate the study by Lira 11 in which 86% of the interviewees stated that they had never been submitted to the clinical examination of the feet. The lack of a care routine and the professionals' limited time available for routine consultations with patients with diabetes may be one of the causes that lead to inadequate evaluation of the feet and registration of the risk classification. In contrast, Hirakawa et al. 17, when conducting a study in the city of Boa Vista/RR with 150 individuals with diabetes, they found a percentage of 46% of patients who claimed to be evaluated annually by an ophthalmologist. In our study, 2.33% of the medical records had fundus examination records. Among the possible causes for this negative result, we can highlight the fact that this exam is not performed in the ESF units and that there is a limited offer of ophthalmological consultations in the public network. In addition, the counter-referral of patients from specialized care to primary care with care reports is not a common practice in the municipality, which negatively affects the recording of information in the patient's medical record.
Still in relation to the SBD guidelines 5, 11.90% of patients were referred to CEAE care. Referral to the CEAE is aimed at patients classified as high and very high risk, with sudden low visual acuity, alterations in the vascular assessment of the feet and/or drug treatment/insulinization that is impossible to perform in primary care. According to our results, it is possible that patients using insulin and without control (17.14%) have an indication for referral, which could contribute to a better control of DM2. It is noteworthy that the lack of a thorough assessment of the patient, the small number of vacancies, combined with the fact that the reference center is located about 80km away from the municipality, are possible limitations to this service.
Cluster analysis pointed to four groups. Cholesterol and triglycerides varied between groups, while BMI was practically similar in all of them, regardless of glycemic control. Among the control patients, two groups had low cholesterol and medium to high triglycerides. Among those who did not have good control, triglyceride values were high in two groups and low in the third. Optimized DM2 control should also consider the adequacy of lipid metabolism and its annual monitoring. Dyslipidemias have a genetic etiology but, in most cases, lifestyle, such as diet and physical activity, have a greater influence and, therefore, the adoption of healthy lifestyle habits should be guided. 18 Cardiovascular diseases are the main cause of death in Brazil. 4 It is known that DM increases the risk of these diseases and that increased levels of triglycerides and LDL cholesterol associated with low levels of HDL cholesterol are also associated with this disease. 18 Thus, based on the data presented, it is possible for services to offer more specific actions and biochemical evaluations to groups of patients who, in addition to DM, have associated dyslipidemia.
Currently, in our clinical practice, there is a great demand for the nutrition service offered, in the municipality, by a professional from the multidisciplinary team that supports the health units. Individual and group nutritional services are a reality in the city. Considering the reduced number of nutritional consultations offered, collective actions and training (matrix support) of other professionals prove to be an interesting strategy for guiding users. The study by Cortez et al. 19 who carried out collective actions with 127 patients with T2DM using public health services in a Brazilian municipality, found significantly better results in glycemic control and in secondary outcomes in the intervention group when compared to the control group (n=111).
This work presents some limitations to be reported. One of them is the fact that the presence of comorbidities such as high blood pressure, kidney and cardiovascular disease, often associated with diabetes, was not evaluated. One of the difficulties in assessing these events is the incomplete filling out of medical records.20 However, we believe that this limitation does not reduce the relevance of the study, since it seeks to reflect the reality of the routine of primary care services. A second limitation was the unavailability of 8.87% of medical records. Despite the loss, we considered the sample to be representative of all patients with DM2 treated at the SUS in the evaluated municipality because the loss was randomly distributed in all health units and the percentage of loss was below 10%, which is acceptable.
Several studies have pointed out the importance of a differentiated approach for patients with DM2. 21,22 In this sense, this work brings an evaluation carried out in a small municipality, which can help to outline new processes in relation to the monitoring of these users. Understanding the profile of patients, using statistical methods that help in grouping them with different profiles, can help in planning strategic actions, defining priorities and maximizing available human resources. It should be noted that 67.90% of Brazilian municipalities have less than 20,000 inhabitants. 23 Most studies are carried out in large municipalities with more resources, whose reality may be different from that observed in small municipalities. This study can contribute to a future and necessary discussion of how municipalities with few resources can reorganize their actions, seeking to overcome the practical difficulties faced in the control of patients with DM2.
CONCLUSION
This study evaluated the profile of patients with DM2 assisted by primary care. Most of the participants were women, elderly, overweight and with a high percentage of people with poor glycemic control. DM2 is a multifactorial disease influenced by a huge range of factors and several difficulties are encountered in the therapeutic process of these patients, both by users and health professionals.
In this sense, new forms of evaluation and different methodologies for characterizing the population, such as the use of statistical methodologies proposed in this work, can help services to better direct their resources and optimize care for patients with DM2, both in defining priorities and actions that contribute to the well-being of users. The data presented here cannot be inferred for other municipalities, however, the results obtained here may also reflect the reality of other municipalities, especially those of small size, and thus make their contribution to public health in other locations.
ACKNOWLEDGEMENTS
“The present work was carried out with the support of the Coordination for the Improvement of Higher Education Personnel – Brazil (CAPES) – Financing Code 001”.
REFERENCES
- American Diabetes Association - ADA. Standards of Medical Care in Diabetes — 2022. Diabetes Care. 2022;45(January):2021–2.
- International Diabetes Federation - FID. IDF Diabetes Atlas [Internet]. 10 ed. Vol. 102, Diabetes ResearchandClinicalPractice. Bruxelas: International Diabetes Federation; 2021. 141 p. Availablefrom: https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf
- Brasil, Ministério da Saúde, Secretaria de Vigilância em Saúde, Departamento de Análise em Saúde e Vigilância em Doenças Não Transmissíveis. Vigitel Brasil 2021 : vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico : estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados . 1 ed. Brasília; 2021.
- Nilson EAF, Santin Andrade R da C, de Brito DA, de Oliveira ML. Costsattributabletoobesity, hypertension, and diabetes in theUnified Health System, Brazil, 2018. Rev Panam Salud Publica/Pan Am J PublicHeal. 2020;44:1–7.
- Sociedade Brasileira de Diabetes - SBD. Diretriz Oficial da Sociedade Brasileira de Diabetes [Internet]. 2022 [acessado em: 2022 May 12]. Disponível em: https://diretriz.diabetes.org.br/
- Brasil, Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Estratégias para o cuidado da pessoa com doença crônica : diabetes mellitus. In: Ministério da Saúde, Secretaria de Atenção à Saúde, Departamento de Atenção Básica – Brasília : Ministério da Saúde [Internet]. 2013. p. 67–80. Disponível em: http://189.28.128.100/dab/docs/portaldab/publicacoes/caderno_36.pdf
- Brasil, Ministério da Saúde. Secretaria de Atenção à Saúde. Departamento de Atenção Básica. Guia alimentar para a população brasileira [Internet]. 2014. 488–490 p. [acessado em: 2022 May 12]. Disponível em: http://link.springer.com/10.1007/978-3-540-72604-3_154
- Brasil, Ministério da Saúde, Universidade Federal de Minas Gerais. Instrutivo De Abordagem Coletiva Para Manejo Da Obesidade No Sus. Brasília : Ministério da Saúde [Internet]. 2021. 154p. [acessado em: 2022 May 12]. Disponível em:http://189.28.128.100/dab/docs/portaldab/publicacoes/instrutivo_abordagem_coletiva.pdf
- Muzy J, Campos MR, Emmerick I, da Silva RS, de Andrade Schramm JM. Prevalenceof diabetes mellitus and its complicationsandcharacterizationofhealthcare gaps basedontriangulationofstudies. CadSaude Publica. 2021;37(5).
- Fiuza MFM, Schuch NJ, Berndt ACC, Marques CT KL. Perfil bioquímico de pacientes diabéticos de um laboratório privado da região sul do Brasil Biochemical profile ofdiabeticpatients in a privatelaboratory in southernBrazil. 2020;1–7.
- Lira JAC, Oliveira BMA de, Soares D dos R, Benício CDAV, Nogueira LT. RiskEvaluationofFeetUlceration in People With Diabetes Mellitus in PrimaryCare. Reme Rev Min Enferm. 2020;24:1–8.
- Brasil M da SS de A à SD de AB. Obesidade - EstratégiasEstratégias para o cuidado da pessoa com doença crônica : obesidade. Vol. 33, Cadernos de Saude Publica. Brasília: Ministério da Saúde; 2014. 2012 p.
- Brasil. Ministério da Saúde. Vigitel Brasil 2019 : vigilância de fatores de risco e proteção para doenças crônicas por inquérito telefônico : estimativas sobre frequência e distribuição sociodemográfica de fatores de risco e proteção para doenças crônicas nas capitais dos 26 estados. [Internet]. Brasília: Ministério da Saúde; 2020. 139 p. [acessado em: 2022 May 12]. Disponível em: https://www.saude.gov.br/images/pdf/2020/April/27/vigitel-brasil-2019-vigilancia-fatores-risco.pdf
- Giesta JM, Zoche E, Corrêa R da S, Bosa VL. Associated factorswithearlyintroductionofultra-processedfoods in feedingofchildrenundertwoyearsold. Cienc e Saude Coletiva. 2019;24(7):2387–97.
- Fiocruz. Determinantes do consumo de frutas , verduras , legumes , arroz e feijão em países de baixa e média renda. 1 ed. Brasília: Fiocruz; 2021.
- Costa ML da, Moraes RB, Vaz DWN, Santos GA dos, Duarte RC da C, Santos Junior JAB dos, et al. Avaliação dos pacientes com Diabetes e Hipertensão em uma Estratégia de Saúde da Família localizada na zona rural do interior do Estado do Pará. Res Soc Dev. 2021;10(3):e2610313025.
- Hirakawa TH, Costa WC, Nakahima F, Ferreira AIC, Ribeiro LB, Ticianeli JG, et al. Knowledgeofdiabeticpatientsusersofthe Health Unic System aboutdiabeticretinopathy. RevBras Oftalmol. 2019;78(2):107–11.
- Mahan LK, L.Raymond J. Krause : Alimentos, Nutrição e Dietoterapia 14aedição. Elsevier. 2017;410.
- Cortez DN, Macedo MML, Souza DAS, Dos Santos JC, Afonso GS, Reis IA, et al. Evaluatingtheeffectivenessofanempowermentprogram for self-care in type 2 diabetes: A cluster randomizedtrial. BMC Public Health. 2017;17(1):1–10.
- Jasmim JDS, Queluci GDC. Studiesondiabeticpatients in primarycare. Revista de Enfermagem UFPE online. 2018 Apr;12(4):1072.
- Aquino JA, Baldoni AO, Di Lorenzo Oliveira C, Cardoso CS, de Figueiredo RC, Sanches C. Pharmacotherapeuticempowermentand its effectiveness in glycemiccontrol in patientswith Diabetes Mellitus. Diabetes MetabSyndrClin Res Rev. 2019;13(1):137–42.
- Torres H de C, Pace AE, Chaves FF, Velasquez-Melendez G, Reis IA. Avaliação dos efeitos de um programa educativo em diabetes: ensaio clínico randomizado. RevSaude Publica. 2018;52:8.
- Instituto Brasileiro de Geografia e Estatística - IBGE. Estimativas da Poulação . 2021 [acessado em 2021 Mar 16]. Disponível em: https://www.ibge.gov.br/estatisticas/sociais/populacao/9103-estimativas-de-populacao.html?=&t=resultados






